What is Degenerative Disc Disease DDD? A Comprehensive Guide

Pain Clues: Could Degenerative Disc Disease (DDD) Be the Cause?
- Do you have leg pain or weakness that spreads from your back?
- Is bending forward painful, while bending backwards brings relief?
If you answered yes, Degenerative Disc Disease or DDD might be behind your discomfort. This issue of Bodi Empowerment delves into DDD: causes, why pain happens, imaging interpretations, and treatment choices.
Treatments for Degenerative Disc Disease
Options range from conservative care (chiropractic, exercise) to surgical interventions like discectomy, fusion, or disc replacement.
Beware: X-rays Don’t Tell the Whole Story
Yes, your doctor found evidence of degenerative disc disease (DDD) on your X-rays or MRI. But here’s the surprise: research shows the severity of DDD visualized on images doesn’t directly tie to your pain level!
- Careful Diagnosis Matters: Doctors must go beyond imaging, using your health history and exam to pinpoint the true pain source.
- Pain Varies Wildly: A person with significant DDD on scans might have mild discomfort, while someone with minor changes suffers greatly.
Understanding Degenerative Disc Disease
DDD refers to wear and tear of the discs between your vertebrae (backbones). Over time, discs may thin visibly on imaging. It’s also known as disc osteoarthritis or spondylosis. Think of it as the ‘wrinkling’ of your spine – a natural part of ageing.
Why Discs Degenerate
- Everyone is Affected: It happens universally, but the timeline varies.
- Genetics Play a Role: Some inherit a tendency for earlier DDD onset.
- Ageing Process: Disc changes begin subtly even in childhood, progressing naturally as we get older
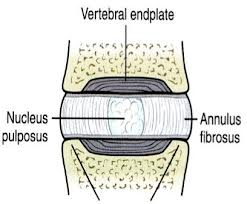
Picture Of A Healthy Disc: Degenerative Disc Disease
Understanding Your Discs: From Healthy to Degenerative
Your spinal discs are more complex than you might think. Let’s break down their structure:
- The Nucleus: The Jelly Center Imagine your disc’s middle is a jelly-like substance called the nucleus.
- The Annulus: The Layered ‘Onion’ The annulus surrounds the nucleus with multiple rings of strong tissue, like the layers of an onion.
- The Endplates: Your Disc’s ‘Mesh’ Floor & Ceiling Picture fine wire mesh covering the bottom and top of your disc – those are the endplates.
How Your Discs Get Nourished
- Childhood: Direct Blood Supply As children, tiny blood vessels tunnel through the endplate mesh, feeding the disc directly with nutrients.
- The Aging Process Sadly, the picture changes in two key ways:
- By age 7: Those blood vessels stop reaching the endplate.[3-5]
- By age 20: The blood vessels through the endplate disappear completely.
Implications of Disc Aging
Without a direct blood supply, nutrients must reach the nucleus by ‘diffusing’ through the jelly and onion layers. This is much slower and less efficient. The effects of this over time are what we call degenerative disc disease. Visible signs on X-rays often start showing up by age 40.
Understanding Disc Degeneration
Internal Pressure and Aging
Your disc bears significant internal pressure to support your body’s weight. Imagine the annulus and nucleus as a balloon filled with water under substantial pressure. However, as you age, a decrease in blood flow, nutrients, and oxygen leads to cell death within the disc.
Decline in Water Content
With fewer cells producing water-retaining molecules, the disc’s water content decreases over time. This reduction in water content results in a decrease in pressure within the disc.
Pressure Redistribution
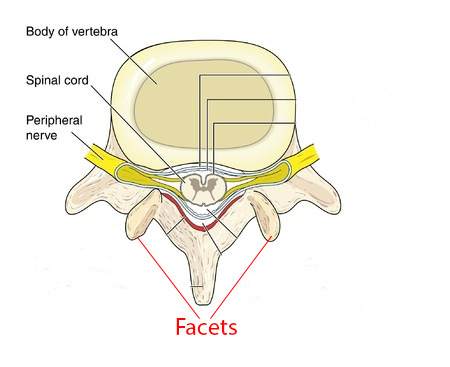
As the disc “deflates,” pressure shifts from the centre to the back, including the annulus and facet joints. This redistribution of pressure can lead to fissures in the annulus and the development of osteoarthritis in the facet joints.
Disc Herniation
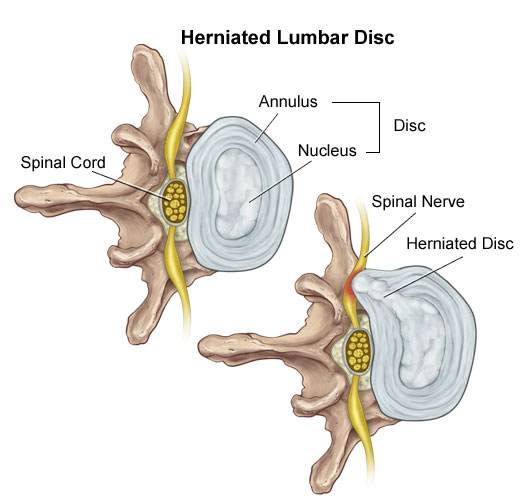
Stage #1 Disc Bulge
- After a few years to a few decades of pressure shifted toward the back of the disc a fissure breaks the many layers of the annulus so that only a few layers of the annulus are left to hold the disc back.
- This allows the nucleus (jelly) to push through the annulus (onion) closer to the edge of the annulus. This is a Disc Bulge ie. the nucleus has been pushed out toward the edge of the annulus.
See Also: Best Treatments To Help Your Lumbar Disc Herniation
Stage #2 Disc Prolapse
- A disc protrusion is like a disc bulge that comes out even more in one focused spot. The disc pushes out as if you had your finger inside a balloon and pushed out.
- A disc protrusion is when the nucleus has pushed through so many layers of the annulus that only one or two layers of the annulus (onion) and a PLL ligament are holding back the nucleus.
- Good news: Severely degenerated discs do not prolapse as there isn’t enough pressure within the disc itself for this to happen.
Stage #3 Disc Extrusion
- A disc extrusion is when the nucleus breaks through the final layers of the annulus and the PLL ligament and pinches on the nerve (spinal nerve).
- In most cases your lower back pain is painful but your sciatica is much worse than your lower back pain.
See Also: Best Exercises For Your Herniated Disc
Vertical Disc Herniation (Smorl’s Node)
- Compression of the spine like lifting very heavy weights, and falling onto your buttock will cause Vertical Disc Herniations in the young.
- When you are young (20 years or under) the annulus is still intact so the weak point becomes the end plate (wire mesh). When you fall and compress your spine severely the annulus is strong enough to withstand tremendous pressure but your weak link is the end plate. The pressure breaks the end plate pushing the nucleus (jelly) into the vertebra below.
- When the nucleus herniates (pushes into) into the vertebra there is more space for the nucleus (jelly) so it’s like deflating a balloon.
- The decreased disc pressure from the disc causes a shift of pressure toward the back of the annulus and the joints (facets) just like a normal disc herniation.
- A Schmorl’s node can be seen on X-ray when the nucleus which has herniated (pushed) into the disc and later on calcifies.
See Also: Your Guide To Disc Bulges, Slipped Discs, Disc Herniations, Disc Protrusion, Disc Extrusions
Why Is My DDD Painful?
Limited Pain Fibers in the Disc
Your disc contains a few pain fibres, primarily located on the outer 1-3 mm of the annulus (the “onion” layer). These fibres typically remain inactive unless the disc is injured.[5]
Onset of Pain
Initially, disc degeneration may occur without causing pain. However, as fissures develop in the outer annulus where the nerve fibres are situated, pain may arise.
Progression of Symptoms
As degeneration progresses, the disc may narrow, develop fissures in the annulus, and potentially form a disc bulge, often leading to persistent pain.
Schmorl’s Node and Pain
The collapse of the end plate, known as a Schmorl’s node, can exacerbate pain by pushing the nucleus (the “jelly” centre) into the adjacent vertebrae, where pain fibres are abundant.
Nerve Growth and Increased Pain
In cases of substantial degenerative disc disease, nerve fibres may grow into the annulus and nucleus, amplifying pain sensations.[6]
Persistent Pain in Disc Herniations
Even in disc herniations, nerve growth into the affected area can contribute to ongoing pain.
Limited Healing Potential
Unlike bones, discs lack the capacity for complete healing following injury, such as a fracture.[2]
Imaging: How To See DDD
#1 X-rays
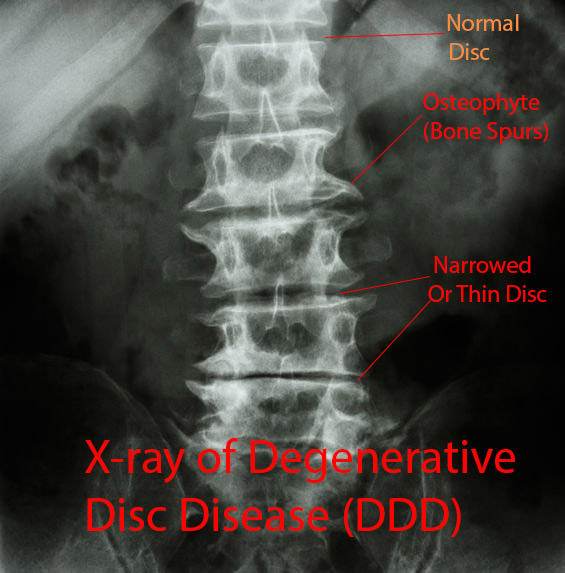
You can see degenerative disc disease on X-rays, CT (CAT) scans and MRI. The most important factors are disc narrowing (smaller), osteophytes (spurs of bone) and disc bulging (seen only on MRI and CT scans)
Often when seen together the radiologist will use the term spondylosis. Most of the time though it may be used to refer to a narrowed disc alone or the presence of multiple osteophytes.
#2 Magnetic Resonance Imaging (MRI)

Magnetic Resonance Imaging (MRI) is the most sensitive tool we have to look at degenerative disc disease. You are looking for disc narrowing, bony spurs called osteophytes, bulging discs and how well the disc is functioning.
MRI Setting T1 and T2
MRI’s have two main settings T1 and T2. The T2 setting shows any tissue that has lots of water in it to show up bright white. The brighter the tissue the more water there is in the tissue.
Normally your disc and spinal cord have a lot of water in so will show up bright white, especially in the nucleus (jelly). As your disc ages, the disc starts to lose water and eventually starts breaking down.
When your disc has substantial degenerative disc disease your disc will no longer look white on a T2 MRI. It will look black since the water has been completely sucked out of the disc. This is called the desiccation of your disc.
#3 Discography

Discography involves injections to try and give you pain in the disc that you think is causing you pain. It’s for people who haven’t responded to non-surgical care and is usually used for planning lumbar fusion surgery.
If your doctor tells you that you need to have a discography you should have serious concerns. First, if you don’t get the surgery it may accelerate disc degeneration and 25% of people are found to have a disc problem when they don’t.[9-10] That’s a huge rate of mistakes.
Remember they are using discography to decide whether they are going to do surgery.
Prevention of DDD
Your mom and dad are the main cause. In other words genetics. Smoking and manual labour are not as important factors for Degenerative Disc Disease. Your parents played the most meaningful part.
The genes that you inherit influence the size, shape and make-up of the vertebrae and disc but also how resilient your disc is.
Degenerative Disc Disease and Disc Herniations
Studies show that if there is a family history of DDD in patients who are diagnosed with a herniated disc before age 21. (Remember you end up with disc herniations as a part of the DDD process)
Frequent Bending, Twisting, Whole Body Vibrations, Smoking and Blood Flow affect
The minor factors which put you at risk for degenerative disc disease are frequent bending and twisting, whole body vibration, [11] smoking from nicotine and impaired blood flow to the disc [12-15] and association of plaques in the arteries called atherosclerosis in the main artery in the lower back [16]
Heavy lifting is associated with disc prolapse but not other areas of degenerative disc disease
Treatment For Degenerative Disc Disease
The golden rule is to always try non-surgical care first. Spinal manipulation by a chiropractor, McKenzie Method approach and lower back stabilization exercises have been shown to relieve pain.[17-18]
Traction and spinal decompression is ineffective for treating degenerative disc disease.
Surgical Options for Degenerative Disc Disease
1. Fusion Surgery (Arthrodesis)
Spinal fusion surgery entails the removal of the nucleus and a significant portion of the annulus. Bone grafts from the pelvis are transplanted to fuse the adjacent vertebrae, creating a single unit.
- Effectiveness and Risks: While fusion surgery can alleviate pain in some cases, it often accelerates degeneration in nearby vertebrae, particularly within a decade post-surgery.[19-21]
- Patient Awareness: Surgeons should provide comprehensive information on the pros and cons of fusion surgery to patients. Failure to do so may raise concerns.
- Concerns about Bone Morphogenetic Protein (BMP): BMP, used as a bone graft substitute, has been associated with potentially life-threatening complications, as highlighted by an FDA public health notification in 2008 [25].
- Comparative Studies: Despite being a standard practice in Europe, studies indicate that fusion surgery may not offer significant advantages over exercise therapy and cognitive therapy in both short and long-term outcomes [26].
2. Total Disc Replacement for Degenerative Disc Disease
Total Disc Replacement involves replacing the problematic disc with an artificial one. However, concerns exist regarding the long-term durability of polyethene [22-23] components and the prevention of adjacent vertebrae wear and tear.
- Motion and Adjacent Vertebrae: Some studies suggest a complete loss of motion at the operated level due to fusion between the artificial segment and the bones[27]. Additionally, evidence does not support the notion that artificial discs reduce degeneration in adjacent vertebrae.
- Risks: Complications such as blood clots or bleeding from injured blood vessels can lead to fatalities following total disc replacement surgery.
Feel free to share your questions, thoughts and experiences in the comments below, and don’t forget to connect with us on Facebook for more updates and tips on improving your health. We’d love to hear your opinions on who you consider the best Toronto chiropractor.
References
1. Boden SD, McCowin PR, Davis DO, Dina TS, Mark AS, Wiesel S. Abnormal magnetic-resonance scans of the cervical spine in asymptomatic subjects. A prospective investigation. Journal of Bone and Joint Surgery—Series A. 1990;72(8):1178–1184.
2. Adams MA & Roughley PJ, What is intervertebral disc degeneration, and what causes it?, Spine 2006; 31(18): 2151-2161.
3. Taylor JR , Growth of human intervertebral discs and vertebral bodies. J Anat. 1975 Sep; 120(Pt 1):49-68.
4. Holm S, Maroudas A, Urban JPG, et al. Nutrition of the intervertebral disc. Solute transport and metabolism. Connect Tiss Res. 1981;8:101–119. doi: 10.3109/03008208109152130.
5. Maximilian Rudert and Bemhard Tillmann, Lymph and blood supply of the human intervertebral disc Cadaver study of correlations to discitis Acta Ofthop Sand 1993; 64 (1): 37-40
References
6. García-Cosamalón J, del Valle ME, Calavia MG, et al. Intervertebral disc, sensory nerves and neurotrophins: who is who in discogenic pain? Journal of Anatomy. 2010;217(1):1–15.
7. Sowa G, Vadalà G, Studer R, et al. Characterization of intervertebral disc aging: longitudinal analysis of a rabbit model by magnetic resonance imaging, histology, and gene expression. Spine.2008;33(17):1821–1828.
8. Prescher A. Anatomy and pathology of the aging spine.European Journal of Radiology. 1998;27(3):181–195.
9. Carragee EJ, Tanner CM, Khurana S, et al. The rates of false-positive lumbar discography in select patients without low back symptoms. Spine. 2000;25(11):1373–1381.
10. Carragee EJ, Don AS, Hurwitz EL, Cuellar JM, Carrino J, Herzog R. 2009 ISSLS prize winner: does discography cause accelerated progression of degeneration changes in the lumbar disc: a ten-year matched cohort study. Spine. 2009;34(21):2338–2345.
References
11. Lötters F, Burdorf A, Kuiper J, Miedema H. Model for the work-relatedness of low-back pain. Scandinavian Journal of Work, Environment and Health. 2003;29(6):431–440.
12. Battié MC, Videman T. Lumbar disc degeneration: epidemiology and genetics. Journal of Bone and Joint Surgery—Series A. 2006;88(supplement 2):3–9.
13. Battie MC, Videman T, Gill K, et al. 1991 Volvo Award in Clinical Sciences: smoking and lumbar intervertebral disc degeneration: an MRI study of identical twins. Spine.1991;16(9):1015–1021.
14. Oda H, Matsuzaki H, Tokuhashi Y, Wakabayashi K, Uematsu Y, Iwahashi M. Degeneration of intervertebral discs due to smoking: experimental assessment in a rat-smoking model. Journal of Orthopaedic Science. 2004;9(2):135–141.
15. Iwahashi M, Matsuzaki H, Tokuhashi Y, Wakabayashi K, Uematsu Y. Mechanism of intervertebral disc degeneration caused by nicotine in rabbits to explicate intervertebral disc disorders caused by smoking. Spine. 2002;27(13):1396–1401.
References
16. Kurunlahti M, Tervonen O, Vanharanta H, Ilkko E, Suramo I. Association of atherosclerosis with low back pain and the degree of disc degeneration. Spine. 1999;24(20):2080–2084.
17. Adams MA & Roughley PJ Spine 2006; 31(18): 2151-2161. What is intervertebral disc degeneration, and what causes it?
18. Beattie P upon etiology, pathophysiology, and lumbar Magnetic Resonance Imaging Journal of Orthopaedic & Sports Physical Therapy 2008; 38(6): 329-340.
19. Song K-J, Choi B-W, Jeon T-S, Lee K-B, Chang H. Adjacent segment degenerative disease: is it due to disease progression or a fusion-associated phenomenon? Comparison between segments adjacent to the fused and non-fused segments. European Spine Journal. 2011;20(11):1940–1945. [PMC free article] [PubMed]
20. Tang S, Rebholz BJ. Does anterior lumbar interbody fusion promote adjacent degeneration in degenerative disc disease? A finite element study. Journal of Orthopaedic Science.2011;16(2):221–228. [PubMed]
References
21. Wu JC, Liu L, Wen-Cheng H, et al. The incidence of adjacent segment disease requiring surgery after anterior cervicaldiskectomy and fusion: estimation using an 11-year comprehensive nationwidedatabase in Taiwan. Neurosurgery. 2012;70(3):594–601.
22. Delamarter R, Zigler JE, Balderston RA, Cammisa FP, Goldstein JA, Spivak JM. Prospective, randomized, multicenter food and drug administration investigational device exemption study of the ProDisc-L total disc replacement compared with circumferential arthrodesis for the treatment of two-level lumbar degenerative disc disease: results at twenty-four months. Journal of Bone and Joint Surgery—Series A. 2011;93(8):705–715.
23. Harrop JS, Youssef JA, Maltenfort M, et al. Lumbar adjacent segment degeneration and disease after arthrodesis and total disc arthroplasty. Spine. 2008;33(15):1701–1707.
24. Center for Devices and Radiological Health. FDA public health notification: life-threatening complications associated with recombinant human bone morphogenetic protein in cervical spine fusion, 2011.
25 Ritzell P, Hagg O, Wessberg P, Nordwall A. Swedish Lumbar Spine Study Group. Lumbar fusion versus non-surgical treatment for chronic low back pain: a multicentre randomized controlled trial from the Swedish Lumbar Spine Study Group. Spine. 2001;26:2521–32.
26. Guyer RD, McAfee PC, Hochschuler SH, Blumenthal SL, Fedder IL, Ohnmeiss DD, Cunningham BW Prospective randomized study of the Charite artificial disc: data from two investigational centers, Spine J. 2004 Nov-Dec; 4(6 Suppl):252S-259S.







This is very helpful,I just read some of what I did not know,or even was told about this disease. Thanks so much
Cervical instability is a condition that can cause a range of symptoms that impact a person’s quality of life. Symptoms of cervical instability may include neck pain, headaches, dizziness, and even issues with balance and coordination. If you are experiencing any of these symptoms, it is important to seek medical attention from a qualified healthcare provider, such as the team at Complete Medical Wellness. Check out this article for more information. Cervical Instability & Cervical Instability Symptoms
Nice! thank you so much! Thank you for sharing. Your blog posts are more interesting and informative. Check out this article for more information. cervical instability treatment
This is a very informative site. Thank you for its creation. I would like to ask your opinion. Will I recover without surgery. First my symptoms then my MRI. History of diskectomy L3L4 6 years ago. Failed Back surgery Syndrome. Pain in lower back chronic. Returned to work after surgery as a nurse but lighter job with no lifting. Unfortunetely lots of desk work and poor posture. Now off work. I had sudden onset of right calf pain 12 weeks ago. Gradually got worse and now unable to weight bear or stand vertical without excruciating calf pain and mild buttock pain. Now my MRI. L3L4 disc desiccation with moderate loss of disc height. Moderate circumferential disk bulge prominent on the left neural foraminal location abutting the exiting L4 nerve root. Moderate bilateral facet joint OA and thickening of ligamentum flavum. Moderate left neural foraminal narrowing. Significant narrowing of left lateral recess.
L4-L5 level disc desiccation with moderate loss of disk height. Small circumferential disc bulge with superimposed right neural foraminal disc protrusion. This is causing marked narrowing of the l ateral recess and mass effect on the exiting L5 nerve root. Moderate narrowing of right neural foraminal. Moderate degenerative changes at this sites. I would appreciate if you can decipher all this for me. Thank you
Dear Doctor,
My Wife recently had a neck pain at right side and consulted doctor, after the x-Ray report stated that ” Minimal Osteoarthritic changes are noted in the cervical spine. There is loss of the normal cervical lordosis. Midly prominent posterior osteophytes are noted at the inferior margins C5,6 and 7 vertebrae. There is minimal postero listhesis of the c7 vertebra. No significant narrowing of the intervertebral disc spaces” doctor suggested to take more calcium intakes,sleeping posture need to improve, usage of good pillow and health food intake. Can you please advice us , any special treatment need to do ? What is root cause ? How to eradicate / minimise potential problem.
Regards
Arvi
Author
Thanks for your question Arvi. First it is quite normal to have degenerative changes at those levels once you are past 40 years of age. https://www.bodiempowerment.com/cervical-disc-herniation-best-exercises-help-sore-neck/
I would recommend the chin tuck exercises. However keep in mind they are not specific for your wife. This is simply a generic exercise that helps most people with a disc bulge in the neck. If the pain gets worse or starts going further down the arm you are getting worse so you must immediately stop.
Hope that helps your possible disc herniation in the neck.
Dr. Nakamura,
Many thanks for an eye opening article. I’ve had 20+ years of progressively worsening lower back pain, as well as bilateral radicular pain. About a year ago, I was taken by surprise and fell, having been caught off guard for the first time, (left side) due to left anterior pain, sudden, stabbing, terminating at the knee. Thank goodness, I had a very good Gyosa when younger and instinct allowed a “break—fall.” (many years of Taekwondo up to L1 dan).
Unfortunately, the next sport I took up was competitive skiing, Moguls and jumps and while I did very well, as you know, many with far beyond my years skiing fall and fall hard. So far, one left TKA, the right knee is also bone on bone, but those are not my problems. The few dozen out of the many, many hundred jumps, off angle, well, you probably guessed the rest.
Last year’s MRI knocked me back, the L-5 is black and now further crowding and compressing both L5-S1 neural foramina which to me confirmed a 3rd Stenosis, Foraminal. No, not a PhD in anything related to medicine. After more than 2 decades looking at these films and reports (much less useful), with study, it is not Quantum Mechanics.
To understand what one can see is one thing, correcting the problem is of course another matter. Born with short pedicles and having been diagnosed years back with Lumbar Stenosis, (congenital and acquired) all could be controlled, the Herniated Disk, (and more) until it came to my facet disease. That last MRI uncovered an 8MM Synovial Cyst in the right lateral recess, right up against the right Facet, again, adjacent encroachment going around the right S1 root in the right lateral recess.
I had been getting along OK, so I thought. Transforaminal Blocks rid me of any sciatic pain for an average of 2-3 years. What I have never been able to control is the lower back pain, which is related not only to the disk herniation (when I say Black L5, I mean on the film, the other disks seem healthy, the L5 seems dehydrated and dead, it is the only way I can explain it, except to say it looks like an image of a Supernova condensing, which will end up with an event Horizon and of course, light will not be able to escape the gravitational pull due to the density and I hope at least a future MRI, will still show the L5 there. Humans cannot compress disks so dense, as to create a black hole on their spine.
Radiofrequency Ablation of both left and right Facets, more accurately, taking out and or confusing the Medial Branch Nerves. They went very well until the last one on 8-Jul-15, right side. Once the skin is pierced and the needle is heated, and sound cranked up, there is no pain when the Medial Branch nerves are hit. I can only describe the sensation as a type of buzzing. Also, an enjoyable feeling. Not so with the last one.
Different doctor than the one treating me over 12 years, he puts up with me, since I will not take any opioid medication and he seems to not be angered by this. Opioids dull the mind and being allergic to NSAIDS, like any signal, pain can be blocked with the mind, with focus. To an extent.
The last “Facet Rhizotomy” (what the doctor’s office I attend calls what I call a Radiofrequency Ablation) did not result in the buzzing. When I was given the signal “let us know when you feel the buzzing as you call it,” there was no buzzing, it felt like a sledgehammer was being slammed against my back, so I shouted, “what the heck was that, it’s not the normal buzz, it seemed like an earthquake and a sledgehammer hitting my back. Not painful, just not normal.
The reply was: “Do not be concerned, we are trying get you more relief.” (SIX MONTHS IS MORE THAN ENOUGH). The doctor’s next words, prior to the second injection, was, “OK, you will feel pain going down your right buttocks, this is normal…” NO IT IS NOT NORMAL I SAID, I’ve had these for 5 years and never felt what you seem to describe as sciatic pain during a simple facet block.
“Calm down, we are trying to help, here goes,” again, the needle is in, the pain shot down my buttocks and began to traverse almost past my knee, SAME exact sledgehammer sound. This time, I think they heard me in the waiting room, when I said: “STOP WHAT YOU ARE DOING NOW, I feel the pain in the buttocks and it kept going, almost past my knee until I yelled, STOP. What is going on?”
The reply: “Oh, you’re not supposed to feel any pain beyond the buttocks, let’s hold and get you dressed and we’ll call to see how you are tomorrow.” Then I am handed a prescription for Oxycodone 15mg tabs ttd. I said, no thanks, you don’t know me Dr. I don’t do narcotics, it’s bad enough they made me take that garbage after my knee replacement for almost a full week. Skin heals.
To end the long story, I woke up in more pain than even I could tolerate and simply laid on the couch with my wife trying to feed me and get me to drink water and me screaming, I am in pain, I’m not hungry. Bad move. 911 had to be called, my BP was 80/50, normally 118/72, pulse 42, normally 65-68. I became dehydrated and still screaming at the ER, no narcotics (yes, I realize now, this is foolish at times), but the ER Doctor gave me Prednisone. A Cortical Steroid and for the first time in 20 years I felt 0 pain. I mean ZERO.
That stupid scale of 1-10, if anyone says, I’m a 10, they should be in the hospital, shot. To me, 6-7 means I’m a mess and can’t make it to the office. 4-5 is normal. Finally visited my PCP, he ran a barrage of tests, which I looked up and realized every single one was testing for RA and only one single test, my CPR, measure of inflammation, was a 6.2 (0-3 normal) and this returned an “I told you, whatever it is you do to deal with your pain, does not mean it is not doing damage.”
BUT, ALL pain was back after that crazy last procedure and in two new areas. Both sides, sciatica, both facets, lower back pain, where only one side would rip me from a deep sleep after 2-3 hours. Both sides returned and two new areas.
My entire back froze, bad upper neck pain, so I assume that is what caused what I have never felt. My entire back was in pain and the left side of my neck was, for the first time in pain, going down my left arm.
That is how I ended up at the ER. Unlike Narcotics, these Oral Cortical Steroids do not in any way affect my mind, how I think. They simply remove pain. However, (OF COURSE) they are not for long-term use and when more than one Neurologist tells you they can operate, but take a few years off, since the shape you are in, guarantees another surgery for Adjacent Segment Disease (after surgery for the Foraminal Stenosis and after a double Fusion), I was close to a profanity.
Based on the added symptoms and research, all I could find is that if someone messes up during a Radiofrequency Ablation and passes through the sacroiliac joint and hits one of the lateral (and not the medial branch nerves) it was weird, the exact same word was used, “sledgehammer,” and nerve damage to the neck. People do have these procedures, for what, I do not know, (however, very precise, not at all like a Medial Branch Fry as I call it at times. I do not know why people have lateral done, I only research what I need to know and I cannot find anything on fixing a procedure that hit the Lateral nerves as opposed to the Medial (assuming this is what even happened) and why EVERY single bit of pain that was being controlled with the injections, (many of which use the same chemical I am now taking orally 5mgs a day), which my PCP said, this is short term, it is possible to come off and go back on and be carefully monitored, but what do you intend to do during the 1-2 months off until you are able to go back on? Turn up the speed on one of those accelerators you like to play with?
Humor is an odd concept to grasp Dr. Apologies for the length of this communication. Thank you in advance should you have any thoughts.
Dean
Author
Thanks for your comments. Sorry to hear that you have had such an awful time. It is helpful sometimes to get a steroid injection, this can make a treatment that isn’t effective to be more effective.
Good luck with your stenosis and disc herniation.
Author
Thanks for your commment Dean. Sorry to hear you went through such pain. You will glad to steroids injections are definitely one of the referrals that I make when appropriate.
Good luck with your lower back pain.
Greetings, Dr. Ken! First of all I’d like to express my gratitude for the information you share with people on this website. Many things were really new to me, like things that bending and stretching forward (trying to get to the toes with palms) can cause a spinal disc bulging. Generally the information you provided I’m sure would help a lot of people! I will share it with everyone I know to be sure they will visit your website or your clinic. I can’t really stress how I’m impressed with what you wrote here! You are the Real Doctor!
Sorry for the long intro, I would really appreciate if you could advise anything specific in my case. I’m 30 yrs old. Recently my back pain increased, once I even couldn’t hold the weight on my right leg (I guess it is called drop foot) and I could not figure out why. But after reading your article about dangers of sit-ups / crunches, I realised that last month this is waht I have been doing everyday to the limit…
I made an MRI and went to our Chiropractor, but due to our town is small she couldn’t really explain completely what was hapening and just read me the MRI results. So I can’t stress how much I would appreciate if you could just explain in simple words what does the following mean:
Description of image:
1. “signs of DDD in L4-S1” (is it even possible, I thought there should be L5 after L4?…),
2. “compression of duramantral space at L4-L5 level (what is this by the way?),
3. “central hernia of L4-L5 up to 6 mm” (does this mean the disc is bulging towards the back or what?),
4. “circular protrusion of L2-L3, L3-L4, L5-S1 (in this case are the disc compressed so they are bulging out of centre?)
5. “Pathalogic change of L5-S1 hyper at T2, STIR and hypo at T1( what does this mean)”
Conclusion: signs of lower back vertebra discs DDD; central hernia of L4-L5, Protrusion of L2-L3, L3-L4, L5-S1, Spondilitis L5-S1.
Yesterday I found your articles and started to perform axercises (laying down on the stomach, sphinx, cobra, bending backwards)and believe me or not, I feel a way better! I’m trying to keep my back straight all the time as it was advised in “Herniated disc part 1” and almost don’t feel any pain. I wish my parrents would tell me all this when I was younger…
anyway, thanks for the info again and sorry for the long post. Hope to see your reply in the nearest future.
Best Regards,
Stan K.
Author
Thanks for your question Stan K.
1. Yes there is a L5 after L4. It’s just a short cut. There is are L45 and L5S1 joints. The radiologist is being lazy and saying that there is the same amount of wear. Best practices would discourage this type of reporting. I have seen a lot worse but I have seen many excellent reports.
2. Dura Mater is the outer covering of the brain that extends down into the spinal cord and even past the spinal cord. It means there is substantial pressure on this part of the extension of the spinal cord. The spinal cord ends at L2 for most people however many nerves go further down the spine. It is these nerves that are being compressed by the disc from #3.
3. This mean you have quite a significant disc herniation that is YES going backwards or posterior.
4. Yes you are right a protrusion is basically a focused bulge of the disc like if you poke your finger into a balloon you have a protrusion into the balloon. A finger is quite focused compared say a soccer ball pushing into a balloon. Hope that makes sense.
5. Means your disc is dried out or dehydrated. A healthy disc has more water content. As it ages and becomes degenerated through injury or the normal aging process people’s disc become dryer. This means the disc is unhealthy and more likely to bulge as the annulus (out part of the disc) is weak and broken in some areas.
Keep doing the exercises.
Hope that helps your degenerative disc disease.
Thank you very much, Dr. Ken. Could not expect more detailed and clear answer.
Wish you all the best & Regards,
Stan K.
Author
You are welcome Stan K.
Dr. What exercises should I do? I have 56 years had MRI conclusion bulging disc low back causing numbness both legs to feet. I probably have degenerative discs. Wondering which exercises to do to not make things worse. Am I going to live the rest of my life with this sensation?
I forget to mention that the mri is showing ddd in l5-s1 disc
Hello sir, I am 32 year old. I am suffering from ddd for the last 3 years. Your article was very informative. I have tried many treatment options but the pain is still there. I feel pain in my left leg also. What is the best exercise for this problem. Is it same as you mentioned for the herniated disc? I am able to do my day to day work but with the pain. Please guide me.
Author
Thanks for your comment Verma. You are right doing the same exercises is helpful for most people.
Try these exercises https://www.bodiempowerment.com/herniated-disc-part-2-the-best-exercises-for-your-herniated-disc/
Hope that helps your disc degenerative disc disease.
Thank you Dr. Nakamura, your advise and information for degenerative disc disease is certainly very helpful and honest. Thank you also for covering every aspect of concern.
Helen
Author
Thanks for stopping by Helen. I hope that helps your degenerative disc disease. Let me know if you have any questions.
Hello Ken – if I may call you so, since I must surely be much older than you, your picture says so.
Just to say that the exercises have really helped and thank you! One question – how long can I stay in any position? i.e. if I am on a cobra stand, can I hold for 3 minutes before lowering myself or should it be same amount of time to prone position and same to cobra position ? What is the maximum duration for holding in any one position? Same question for back bending – can I hold longer or is it not advisable?
Trust I have phrased it well so that you know exactly what I mean. Thank you Ken.
Helen
Author
Thanks for your comment Helen. When doing the Cobra exercise you should hold it for a several seconds (3-5 seconds) than go back down. Do the exercise 8 times and follow-up every 2 hours when you are having pain.
Hope that helps your degenerative disc disease.
This is a great blog! Hi. I have being seeing a physio for two years. My pain wasn’t getting better so she referred me for an extension and flexion x ray. This showed ‘mild cervical instability of c2/3 and c3/4. An orthopaedic registrar saw it and said I needed a neurosurgery consult. My GP wrote a referral but sent it to medical neurology it seems by mistake. A neurosurgeon never saw it. The neurologist decided I didn’t need any further assessment despite the x ray findings and recommendation of the orthopaedic registrar and passed a referral on to a headache clinic!
I have neck pain and severe pain at back of head. Sharp pain at times when my neck seems to catch. I have had periods where I get pain radiating down my left arm too. I also have lower back pain and intermittent sciatica for which I have had no investigations.
Would the neck x ray have shown up any arthritis or degenerative disease along with the instability if it was there? Could the neck problems and lower back problems be linked? Do you think I should ask to be re referred to either a neurosurgeon or an orthopedic surgeon?
Author
Thanks for your comment Skye. Quite often a GP will send their patients to see a neurologist first, who doesn’t do surgery to see if they need a neurosurgeon. Since your neurologist looked at the X-ray (at least they should have) they would know that there is mild cervical instability and should refer you for rehabilitation of your neck. If you got the proper rehabilitation exercises and treatment exercises from your physiotherapist it would have gotten better by now. If they only sent you for X-rays after 2 years then the physiotherapist is not providing the correct treatment and investigations on a timely basis.
You should than find an another physiotherapist or a chiropractor that is knowledgeable about rehabilitation.
X-rays show degenerative disease and some types of arthritis but won’t show herniated discs which a part of DDD (Degenerative Disc Disease). You need an MRI to show herniated discs. Sounds like the problem is mainly related to the instability. Neck problems don’t often cause lower back problems but lower back problems quite often cause neck and upper back problems. So the answer is no.
You should go to a competent physiotherapist or chiropractor first. A neurosurgeon or orthopedic surgeon are both equally qualified but go with the person with experience. The person that does neck surgery everyday. Their titles don’t matter. Experience counts too. Would you like to the patient for the surgeon who is doing his first neck surgery.