Why Your Night Guard Isn’t Fixing Your TMJ (And What the Research Actually Shows)
If you’re wearing a night guard every night and your jaw still hurts, you’re not alone. Across Toronto, many patients are told that a Splint or Night Guard will solve their TMJ pain, but for most people with ongoing symptoms it only addresses part of the problem. For a full overview of TMJ causes and treatment options, see TMJ Pain: Causes, Symptoms, and Treatment.
While night guards can be helpful in specific situations, they are not designed to correct the underlying causes of most chronic TMJ disorders. To understand why your symptoms persist, we need to look at what a night guard can do—and what it simply cannot address.
What a Night Guard Is Actually Designed For
A night guard (occlusal splint) is a protective device, not a corrective one. Its primary functions are to:
- Reduce grinding forces on the teeth (especially in people with bruxism-grinding)
- Decrease pressure inside the TMJ
- Temporarily alter bite mechanics
- Protect enamel and dental work from wear
These effects are helpful, but they are limited.
Research shows that splints can reduce symptoms in short‑term inflammatory TMJ conditions, particularly when bruxism is severe or the joint is acutely irritated. However, they do not correct the deeper biomechanical or neurological issues that drive most persistent TMJ pain. For a broader look at conservative TMJ care, see TMJ Pain: Causes, Symptoms, and Treatment.
A night guard cannot:
- Restore proper cervical spine function
- Correct muscle imbalance around the jaw, neck, and shoulders
- Improve forward head posture from long hours at a desk or on devices
- Regulate stress‑driven clenching
- Reduce long‑standing neuromuscular tension or central pain sensitivity
If the root cause of your TMJ pain is not primarily dental, the appliance will not resolve it.
The Real Drivers of Ongoing TMJ Pain
In clinical practice, long‑lasting TMJ pain is rarely caused by the teeth alone. The jaw is part of a larger system involving the neck, posture, muscles, and nervous system. When these areas are not evaluated, treatment becomes incomplete—and symptoms persist.
Below are the most common contributors to chronic TMJ dysfunction.
1. Cervical Spine Dysfunction (The Jaw–Neck Connection)
The jaw and upper cervical spine are tightly linked through shared nerves and muscular chains. When the neck is not functioning well, the jaw is almost always affected.

Forward head posture—common with prolonged computer and phone use—increases strain on:
- The masseter: A jaw muscle
- The temporalis: A jaw muscle on top of your temple.
- The suboccipital muscles: Neck muscles
This added load changes how the jaw moves and how the TMJ absorbs force, often contributing to neck pain and headaches as well as jaw pain. To learn more about this relationship, see Neck Pain and TMJ: How They’re Connected.
Without addressing the neck, jaw symptoms often plateau or return. If you’re dealing with persistent neck issues along with TMJ pain, you may also benefit from the information in Neck Pain Treatment in Toronto.
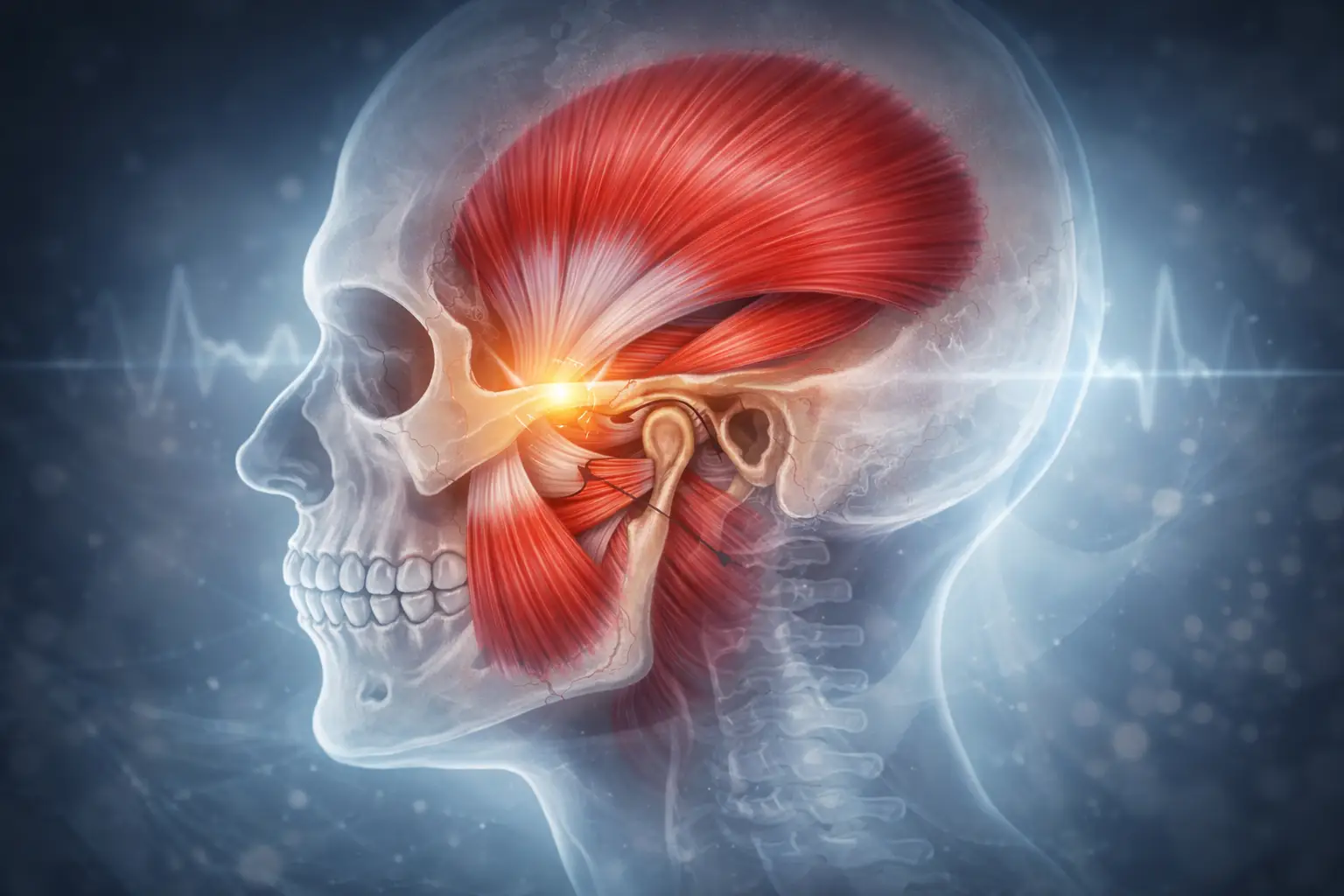
2. Myofascial Overload and Stress‑Clenching
Chronic clenching is not simply a dental issue. It is a stress‑regulated motor pattern controlled by the nervous system.
The trigeminal nerve (which controls jaw muscles) interacts with:
- The sympathetic “fight‑or‑flight” system
- Sleep regulation
- Concussion history
- Chronic pain sensitivity
A night guard can protect your teeth, but it cannot change the neurological pattern driving the clenching. Addressing this often requires a combination of breathing work, relaxation strategies, and targeted muscle treatment.
If you’ve had a concussion and notice that your jaw tension and anxiety worsened afterward, you may also find Concussion Rehabilitation helpful.
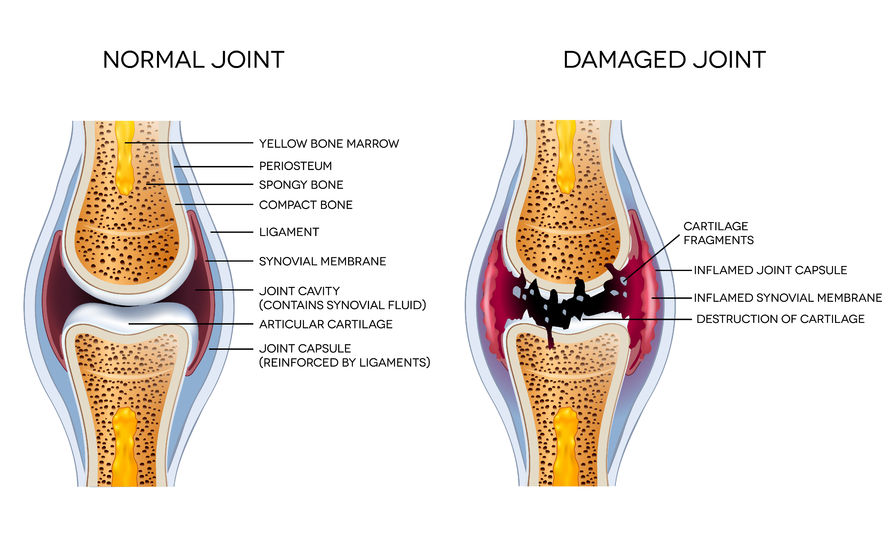
3. TMJ Disc Displacement
When the disc inside the TMJ shifts forward, patients often experience:
- Clicking
- Popping
- Locking
- Pain with opening or chewing
If the disc is displaced, a splint alone rarely resolves the issue. Treatment must focus on restoring joint mechanics and improving muscular control—not just altering the bite. This usually involves specific exercises, manual therapy, and improving neck and shoulder mechanics alongside jaw work. For a structured overview of how TMJ is assessed and treated, see TMJ Pain: Causes, Symptoms, and Treatment.
4. Central Sensitization
When pain becomes long‑standing, the nervous system can become more sensitive, amplifying pain signals even when the joint itself is less inflamed. At this stage, local treatments like night guards are not enough.
The entire system needs to be addressed through:
- Education about pain and the nervous system
- Gradual, graded exposure to movement
- Better sleep and stress management
- Coordinated care that looks beyond just the jaw
If your pain feels “out of proportion” to what imaging or dental exams show, this broader view is especially important. You can read more about whole‑body, evidence‑based care in Chiropractic Toronto – Evidence‑Based Care.
When Night Guards Do Provide Value
Night guards are not useless—they simply have a specific role. They are most effective when:
- The TMJ is acutely inflamed
- Bruxism is severe and damaging the teeth
- There is clear bite instability after dental work
- They are used as part of a comprehensive treatment plan
In these situations, a night guard can reduce load on the joint, protect enamel, and provide short‑term symptom relief while you address the underlying issues through targeted treatment of the jaw, neck, and nervous system. For guidance on what a full TMJ plan can look like, see TMJ Pain: Causes, Symptoms, and Treatment.
The key point: a night guard should be one component of care, not the entire strategy.
What a Proper TMJ Assessment Should Include
A thorough TMJ evaluation goes far beyond looking at the teeth. A complete assessment should examine:
- Jaw range of motion and how smoothly the joints track
- Cervical spine mobility and alignment
- Muscle tension and trigger points in the jaw, neck, and shoulders
- Posture and head position (especially forward head posture)
- Headache patterns and their relationship to jaw and neck movement
- History of trauma or concussion
- Stress levels and sleep quality
When these factors are evaluated together, treatment becomes targeted, effective, and long‑lasting instead of focusing only on adjusting or remaking splints.
Why This Matters for Toronto Patients
Many patients who come into the clinic have already:
- Seen a dentist
- Tried a night guard
- Tried massage
- Tried medication
Yet no one has assessed the jaw–neck connection or the neuromuscular patterns driving their symptoms.
Persistent TMJ pain is rarely a simple dental problem. It is a biomechanical, muscular, and neurological issue that requires a broader, more integrated approach. .
From there, the next step is a detailed in‑person assessment so your jaw, neck, posture, and nervous system can all be addressed as part of one coordinated plan.