Managing Disc Bulge: Effective Strategies for Pain Relief

Do you have a disc bulge that is causing you incredible pain in your lower back?
Does your disc bulge give you sciatica or pain down your leg?
Have you wondered what’s going on in your lower back to cause all this pain?
In this issue of Bodi Empowerment, I go over what’s going on with your disc bulge, the cause of your pain and what kind of treatments are best for you. In other words, I act as a guide to help you decide what to do.
Disc herniations, or disc bulges occur when the disc that is found between vertebrae in the spine is damaged. Most of the time the damage occurs in stages.
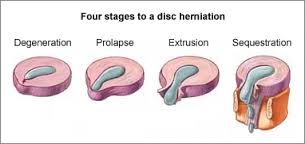
Here are the four stages of a disc herniation or disc bulge:
- Disc Bulge
- Disc Prolapse
- Disc Extrusion
- Disc Sequestration
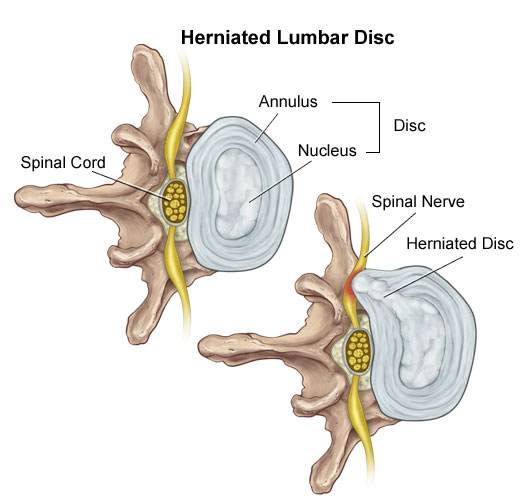
Think of the disc as a flat hard onion with strawberry jelly inside. The jelly is the nucleus while the onion layers form circular layers of hard cartilage called the annulus.
Disc Bulge
If you were to damage the annulus (onion) enough the disc gets to a point that when you bend forward, you pinch the front of the onion so it starts to bulge the onion at the back by pushing the nucleus (jelly) backwards.
This is called a disc bulge. For most of you, there is no pain but for some of you, there can be considerable lower back pain and even sciatica from this small disc bulge.
Disc Protrusion
A disc protrusion is like a disc bulge that comes out even more in one focused spot. The disc pushes out as if you had your finger inside a balloon and pushed out.
Most of the layers of the onion (annulus) have been damaged but the jelly (nucleus) is under considerable pressure. The jelly (nucleus) squeezes through the layers of the annulus (onion) with the few intact layers of the onion (annulus) and the PLL (posterior longitudinal ligament) holding the jelly from spilling out. The disc is still contained by the annulus and PLL ligament. ie the balloon hasn’t popped.
Disc Protrusions usually cause quite a bit of lower back pain and often times sciatica. Many of you, with disc protrusions, on the other hand, have absolutely no pain. There is no clear reason. A study found that 40% of people with no pain whatsoever had disc protrusion confirmed by MRI (Magnetic Resonance Imaging Machine) [1]
The trick is not to let your doctor diagnose you based on just an MRI. An MRI that shows a disc protrusion by itself is not a diagnosis. It’s what a normal person with no pain can have. Make sure there is other evidence!
Disc Extrusion
Disc Extrusion is a disc bulge so large that it breaks through the last layers of the onion (annulus) and the PLL ligament pushing into the area of the spinal cord. ie. The balloon has popped. If you have an extrusion you likely have a tremendous amount of pain leg pain and usually some lower back pain.
Surprisingly when a group of normal people with no pain were scanned with an MRI 18% were found to have disc extrusions (severe disc herniations). [1]
When you have a disc extrusion chances are the extrusion is likely causing your pain as it’s so large.
Disc Sequestration
Disc sequestration occurs when a piece of your jelly (nucleus) that breaks through the onion (annulus) and the PLL ligament has now broken off and moved away further into the spinal cord area. When you have a disc sequestration you have a tremendous amount of leg pain and some lower back pain.
Smaller Is Better: Disc Bulge
Disc Herniations or slipped discs are better if they are smaller, right? You will have less pain right? Yes except when they give you pain. Remember all those normal people with no pain with all kinds of slipped discs? They had disc bulges, disc protrusions, and disc extrusions and even disc sequestrations with no pain.
On the other hand, even with a small disc bulge, you can get a lot of pain and even sciatica with no pressure on the nerve. So smaller isn’t always better.
Bigger Is Better: Disc Bulge
Sometimes bigger is better. Most people like you with disc extrusion and sequestration have lots of pain. The fact is these painful extrusions while more painful usually shrink with time. It takes about a year but with the shrinking of the herniations, the pain does decrease.[2-5]
Disc Herniation: Disc Bulge Treatment
#1 Stop Aggravating Yourself
Half the problem why people don’t get better is that they continually aggravate their lower back and their slipped discs. Learning to lift properly, sit properly and even stand over the sink while brushing your teeth properly can help you avoid the pain.
Even Yoga exercises such as the downward dog can aggravate the lower back, Pilates and even your basic abdominal crunch have been shown by Dr Stuart McGill to increase the pressure in the disc beyond its safe limit.
If you want to find out how to stop aggravating your lower back, click the link below.
See Also: Slipped Discs: Best Self-Treatments To Help Your Lumbar Disc Herniation
#2 Exercise For Disc Herniations / Slipped Discs
For complete instructions on exercises for slipped discs click the link. Best Exercises For Your Slipped Disc
#3 Chiropractic Adjustments For Disc Bulge
A major research paper showed that people who have had lumbar disc herniations who have failed at least 3 months of medical management, including treatment with analgesics, lifestyle modification, physiotherapy, massage therapy, and/or acupuncture, should consider chiropractic spinal manipulative treatment, followed by surgery if unsuccessful. [6]
I would also add that I would try 3 different chiropractors as the competency level varies from person to person. Like any profession including medical doctors and physiotherapists, there are the good ones and bad ones.
See also: 6 Things You Should Look For In A Chiropractic Clinic
#4 Acupuncture For Disc Bulge
Acupuncture is helpful for Slipped Discs in the neck and the lower back.[7-8]
#5 Injections
In a study of two different groups getting treatment for lumbar disc herniations, the group getting chiropractic manipulation had 76.5% of the people improve while the group getting the nerve root injections improved by 62.7%.
After a month, the chiropractic spinal manipulation group had a 60% reduction in pain compared to the nerve root injection group, which had a 53% decrease in pain. Keep in mind the nerve root injection group seemed to be worse to start with compared to the spinal manipulation group.
See Also: Chiropractic Spinal Manipulation Vs. Nerve Root Injections for Lumbar Disc Herniations
Epidural injections are also helpful for lower back pain and the radiating pain down your leg.[8]
#6 Surgery
#1 Discectomy
There are two types of surgery available for slipped discs. Discectomy and spinal fusion. This surgery involves cutting out the piece of the disc that is protruding out and pushing on the spinal cord or nerve.
Discectomy is relatively simple compared to spinal fusion. You have a much better chance of success with discectomy if your MRI shows that your disc herniation is greater than 7 mm thick and correlates well with your neurological exam and nerve conduction studies.[9] If your lower back pain is greater than your leg pain discectomy will not likely work very well for you.[10]
#2 Spinal Fusion
Spinal Fusion removes the disc herniation, jelly (nucleus), and most of the annulus (onion). Bone from the pelvis is then transplanted where your disc was so that the two vertebrae become one.
What Treatment Should You Do?
You should do at least 3 months of therapy when you have a slipped disc before even considering surgery or injections. Start by not aggravating your lumbar disc. You need to modify how you bend forward, lift and even pick up your socks.
See Also: Disc Herniation: Best Self-Treatments To Help Your Lumbar Disc Herniation
If you have trouble sleeping at night you can take painkillers to help you get a better sleep. Don’t stay in bed though. When you have excruciating pain you should only have bed rest for a maximum of two days total.
Next, try chiropractic or physiotherapy with someone who also does acupuncture. Make sure it’s not with somebody who knows how to do 20 acupuncture points. Be patient with them as disc herniations can be difficult to deal with.
Attend regularly 3 times a week for at least a month. Make sure they change the treatments to find what works best for you. If they keep doing the same thing each visit but you are improving that is fine, but if you aren’t improving then it’s time to find a new chiropractor.
If you don’t get any better after a month change to a different chiropractor. I recommend trying 3 different chiropractors as different chiropractors have different training.
If you plateaued or haven’t improved at all then it’s time to get a nerve root injection or an epidural injection. Make sure it’s with a person that does this every day. An emergency room doctor or family physician only does this procedure once in a while. It’s better to get someone more experienced.
When conservative care has been completely exhausted then it’s time to consider surgery. Discectomy is more conservative than spinal fusion and recovery is much quicker. You should consider discectomy surgery if you have :
- Foot drop that is getting worse.
- Any other neurological symptoms that is getting worse like your reflexes, sensitivity
- Bowel or Bladder Symptoms (loss of your poo and pee function). : This is an emergency you should go to the hospital right away.
- If you have a disc protrusion or that is 8 mm or larger that correlates well with a neurological exam, and Nerve conduction tests.
- Leg pain is worse than your lower back pain.
Beware of the surgeon who wants to operate on a small disc bulge. There are too many unnecessary surgeries in the USA especially spinal fusion.
Spinal fusion is considered when your lower back pain is worse than your leg pain
Tell us what you think in the comments below and like us on Facebook. This Toronto Downtown Chiropractor will answer all questions in the comments section.
Research
1. Weishaupt D et al. “MRI of the lumbar spine: Prevalence of intervertebral disc extrusion and sequestration, nerve root compression and plate abnormalities, and osteoarthritis of the fact joints in Asymptomatic Volunteers.” Radiology – 1998; 209:661-666
2. Maigne JY, Rime B, Delignet B. Computed tomographic follow-up of 48 cases of nonoperatively treated lumbar intervertebral disc herniation. Spine 1992; 17:1071-1074.
3. Ikeda T, et al. Pathomechanism of spontaneous regression of the herniated lumbar disc: histologic and immunohistochemical study. J Spinal Disord 1996;9:136-140.
4. Ahn SH, Ahn MW, Byun WM. Effect of transligamentous extension of lumbar disc herniations and their regression in the clinical outcome of sciatica. Spine 2000; 25:475-480.
5. Komori H, Shinomiya K, Nakai O, et al. The natural history of herniated nucleus pulposus with radiculopathy. Spine 1996; 21:225-229.
Research
6. McMorland G et al.Manipulation or microdiskectomy for sciatica? A prospective randomized clinical study. Journal of Manipulative & Physiological Therapeutics 2010; 33: 576-584.
7. Wu, Yao-chi, Jun-feng Zhang, Yi-jun Sun, Cheng-fei Huang, Ping Shao, and Gui-zhen Liu. “Clinical study on electroacupuncture for cervical intervertebral disc herniation.” Journal of Acupuncture and Tuina Science 11, no. 6 (2013): 371-374. – See more at: http://www.healthcmi.com/Acupuncture-Continuing-Education-News/1249-acupuncture-found-superior-to-drug-for-neck-disc-pain#sthash.vD0pNepM.dpuf
8. Wang HeshanNon-Surgical Therapy For Prolapse of Lumbar Intervertebral Disc. The Journal of Traditional Chinese Medicine
9. Parr AT, Diwan S, Abdi S. Lumbar interlaminar epidural injections in managing chronic low back pain and lower extremity pain: a systematic review. Pain Physician 2009;12:163-188.
Research
10. Carragee EJ, et al “Clinical outcomes after lumbar discectomy for sciatica: The effects of fragment types and annular competence” J Bone Joint Surg Am – 2003; 85(1):102-108
11. McMorland G et al.Manipulation or microdiskectomy for sciatica? A prospective randomized clinical study. Journal of Manipulative & Physiological Therapeutics 2010; 33: 576-584.






My chiropractor is recommending spinal decompression for L4&L5 9 mm disc bulge . What are your thoughts on this therapy. It would be an out of pocket expense of $5000.00
Author
Thanks for your question Cindy. $5000 in my opinion is excessive. Traction is the same as decompression. Both can vary the amount of pressure and do intermittent or constant traction. I would find a place that does traction and see how you do for your disc bulge. Generally speaking intermittent traction is better for a disc bulge.
Hope that helps your disc bulge. If you need any more help, I will do my best to help you in any way I can.
I like what you guys are up too. This type of clever work and coverage!
Keep up the amazing works guys I’ve included you guys to blogroll.
Hi Dr Nakamura,
I’m 38 years old and have been having severe back pain for 3 months. I had an MRI which showed a 17mm herniated disc and my doctor has recommended surgery. I’m on a waiting list and have been doing physiotherapy and chiro but my symptoms are worsening. The pain is mainly in my lower back but also radiates down my left leg and groin and shoots up my back. I’m at the point where I can barely walk and I can’t straighten my back without severe pain. I don’t know where to go from here because it’s getting worse by the day. Any advice would be greatly appreciated!
Thank you
Author
Thanks for your question Vicky, when your disc herniation is 17mm yes the disc herniation is most likely causing the pain and usually anything over 8mm is considered a candidate for surgery in Canada. Not sure where you are from but your question about worsening symptoms is concerning!! At this point chiropractors and physiotherapist are not likely to affect it much. I would get a second opinion right away to determine if this is more of an urgernt case with more immediate care needed. This is an opinion and not a recommendation. That’s the best I can do.
Hope that helps.
So I been having lower back pain throbbing/burning/stabbing and it shoots down my quads Into my groin area down into my legs so I got a MRI done and it showed I have a disc bulge in L5-L1 2MM my question is with it being only 2MM could it cause that much pain in my lower back?
Author
Hi Dave, Thanks for your question. Your MRI was taken lying down which puts less pressure on the vast majority of people’s lumbar discs. The only exception is if you have hyperlordosis, which is a very arched spine when standing or lying. So while sitting or standing or bending forward the lumbar disc for most people has substantially more pressure. From lowest pressure to highest pressure on the disc is: lying, standing, sitting, bending forward then lifting something off the floor. So the heavier an object you lift the more pressure on the disc. In essence you can have substantial pain from an MRI that shows only 2mm disc herniation.
However, the disc may not be the cause. Your health care practitioner like a chiropractor or medical doctor would have to do a thorough exam and history to determine if what is found correlates to your MRI. A common finding with disc herniations in the history is if coughing, sneezing or bearing down to go to the bathroom aggravates your lower back. Doing a neurological exam to see what nerve is trapped and correlating that to the L5S1 disc would be helpful. Your chiropractor would have to determine this to find the right answer.
Keep in mind this is an opinion and not a recommendation as I have not examined you. Best you find a great chiropractor or physiotherapist to help you out. I find it’s not the profession but the person that treats that is the most important.
Hope that helps. I always do my best to to give you useful answer.
Greetings Dr.
I really appreciate the time and effort that you have taken to answer our questions.
I recently suffered a disk herniation from deadlifting. I sought medical care and had an MRI done. The MRI found that I had suffered from 8mm disk herniation on my L4/L5; Is this considered a large herniation? Are there any journal articles that state what the range is for a herniation to be considered large?
I also wanted to know the stats and literature around the likelihood of reherniating my disk. However, the only data and research that I found are in regards to the probability of reherniation after microdiscectomy and lumbar discectomies.
Could you send me a journal article that discusses the probability of suffering a disk reherniation prior to surgery? Basically, I want to know if I am more likely to suffer a herniated disk because of an initial herniation without first undergoing surgery.
Thank you,
Author
Thanks for your question Sam. Yes an 8mm disk herniation is considered large. Large enough that many studies point out that 8mm is the minimum amount of a disc herniation before they would consider surgery.
As for the stats are 1-21% according to many studies.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3996348/
I have personally treated many people after getting discectomies, and many people that have no surgies suffering a reherniation. The link is there for you to look at.
Hope that helps.
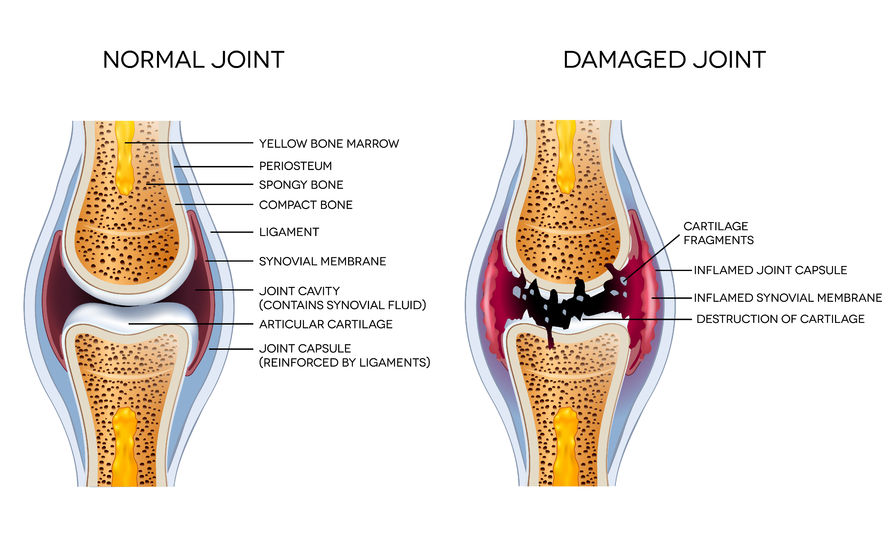
Hi Dr. Nakamura. First off, I want to thank you for writing an article that the general public can understand. I had received the results of my cervical MRI and was at a complete loss of understanding until I found this article. I was diagnosed with JRA (Juvenile Rheumatoid Arthritis) at the age of 9 and was told by several rheumatologists throughout my life to avoid surgery at any cost due to the rheumatism. Anyway, my current rheumatologist just told me that my current MRI said I have 2 herniated discs & is referring me to a pain management specialist/anesthesiologist, in order to get a shot in my neck. I get the cortisone injections in my knees, so, I’m quite used to them. I once went to a chiropractor and had a bad experience, when I was in my early 20s) and I am very hesitant to go back to a new one. I understand that there are good and bad chiropractors, but my rheumatologist feels that with my condition, manipulation of the joints would not be a good idea. Sorry this is so long. I have 2 questions, if I may. After reading your article, I now understand that one of my disc herniations is at the extrusion level, as my diagnosis says, “broad based 0.26 cm central herniation of the disc indenting the anterior thecal sac and contacting the cord at c2-c3.” C3-c4, c4-c5 & c5-c6 do not say anything like that. Question #1: is .26 cm a small, medium or large herniation? Question #2: which of the following is the second herniation? -“posterior spur and disc complex effacing the anterior thecal sac and right uncinate spurring producing moderate right foraminal narrowing at c3-c4”, “posterior spur snd disc complex effacing the anterior thecal sac and bilateral uncinate spurring producing mild bilateral foraminal at c4-c5”, or, “posterior spur and disc complex wffacing the anterior thecal sac and producing mild cord flattening and right uncinate spurring producing moderate left foraminal narrowing at c5-c6?” The only differences I can see are in the uncinate, whether it be right or bilateral, the forminal, whether it be moderate right narrowing, mild bilateral, or or moderate left narrowing. (I have actually no idea what any of this means) Also the last one says mild cord flattening, this does not seem to fit in with your explanation of a herniated disc. Would you please, as you so eloquently did before, use layman’s terms and explain. Thank you so much in advance. Amanda
Author
Thanks for your question Amanda.
Answers to your question.
1. 0.26cm or 26 mm is no considered a large disc herniation. It would be considered small to medium.
2. Keep in mind your symptoms are more important than what the MRI says. While you may have “moderate right foraminal narrowing” you don’t actually say what your symptoms are except to say that you got an injection in your neck. Often times MRI finding and symptoms don’t correlate that’s why your symptoms are so important.
So, without the proper information, I can’t give you an informed opinion. To answer your question the area of most interest is at C34 where there is a moderate narrowing of the foramina which means that the nerve that comes out of between two vertebrae is narrowed so there can be pinching of the nerve. Just because there is a narrowing of the hole for the nerve doesn’t mean there is pinching of the nerve. That’s why there is no correlation between symptoms and MRI according to many research studies.
“posterior spur and disc complex effacing the anterior thecal sac and bilateral uncinate spurring producing mild bilateral foraminal at c4-c5”
This means that bones have started to change shape so that it is sticking out. Combined with the disc that is sticking out these together are which is pushing on spinal cord mildly.
“right uncinate spurring producing moderate left foraminal narrowing at c5-c6?” This doesn’t make sense unless the spur is gigantic going across from right to left. The MRI would indicate that the spur is gigantic if this was true. More likely this is not true. Likely it was the “left uncinate”. However, you only gave me bits and pieces of the MRI and not the whole MRI so I don’t have the whole context of what was written.
Hope that helps. The above is an opinion and not a recommendation.
If you have any more questions regarding your neck, this Toronto Chiropractor will do his best to give you a good answer to your question.
Hello dr.ken nakamura
Im Noman from pakistan i haveing a lower back pain and in leg specialy when standind or walking i do MRI
MRI report .straightening of lumbar curve.
Diffuse disc bulge more towrds in right side is seen at L5 – S1 level causing effacement of anterior thecal and lateral recesses.
Facet joints and ligamentum flavum hypertrophy and desiccatory changes are seen at the same levels.
Vertebare: ( Normal)
Vertebral marrow: (Normal)
Posterior neural arches:(Normal)
CONCLUSION: diffuse disc bulge more towards right side at L5 S1level causing effacement on anterior thecal and lateral recesses.
Dear doc. first i consult with Neuro doc he suggest me to opprate thn i consult with Orthpadic doc he say aviod opprate start meddicine he gave me pain killers 3 types and 2 types calcium medi. I use 1 month but no improvement i consult with therapist for 1 week but failed. Know dear Doc told me what should to doo how to get rid with that.
Thanks n regard Noman shauakat
Author
Thanks for your question Norman. As for surgery, the rule is that you always do conservative therapy first. However, keep in mind I have not examined you. At the same time, you are getting two different opinions on the same condition. These exercises in this article will likely help you. Here it is: https://www.bodiempowerment.com/herniated-disc-part-2-the-best-exercises-for-your-herniated-disc/
The above is an opinion and not a recommendation.
Hope that helps your slipped disc. If you have any more questions for this downtown Toronto chiropractor just let me know and I will do my best.
Dear Sir,
My Name is Ramesh. I am 36 old and working in private sector as desktop engg i.e My daily sitting on chair almost 8 to 10 hrs.
i have lower back pain and neck pain since last 4 to 5 months.
In neck pain sometimes it will pain my head as well.
Back pain is very critical it will start when i sit more than 15 to 30 minutes and then pain continues.
When i sleep there will no pain in back.
i did physiotherpy for one month but still no improvmnet.
please suggest how i can treat further to solve my back and neck pain problem .
Which Dr will help me in this problem (orthopedic/neurologist/rheumatologist…etc)
Will Acupuncture help to reduce back pain ?
shall i use back belt ?
MRI REPORT:
Imaging sequences:
===================
SE T1W Sagittal and axials FSE T2W sagittal & axias
Findings:
==========
1. There is loss of normal T2W bright signal in L2-L3 intervertebral disc suggestive of partail disc dessication.
2. Rest of the vertebral bodies are normal in height morphology and signal charactristics
3. Spinal cord and cauda equina are normal in signal intensity
4. spinal cord ends at L1-L2 level
Degenerative disc disease of the lumbar spine with changes at varous lavel as described below in decreasing order of severity.
At L2-L3 Level :Diffuse disk bulge is noted identing the thecal sac ,narrowing bilateral neural foramina and abuting left exiting nerve root.
Left extra-foraminal annular tear and mild ligamentum flavum thickening is noted at this level.
At L3-L4 Level :Central and bilateral paracentral disc buldge is noted identing the thecal sac, narrowing bilateral neutral foramina without any nerve root compression.
AT L4-L5 Level :Central and bilateral paracentral disc buldge is noted identing the thecal sac, encroaching bilateral neutral foramina just abuting bilateral existing nerve root.
At L5-S1 Level :Central and bilateral paracentral disc buldge is noted identing the thecal sac, encroaching bilateral neutral foramina just abuting bilateral existing nerve root.
Right annular tear is noted ar this level.
Lumar canal diameter at disc level are as follows.
L1-L2=15 mm
L2-L3=12 mm
L3-L4=11.6 mm
L4-L5=11.5 mm
L5-S1=11.7 mm
Author
I did physiotherapy for one month but still no improvement.Sorry to hear that.
please suggest how I can treat further to solve my back and neck pain problem. You can do these exercises here. https://www.bodiempowerment.com/herniated-disc-part-2-the-best-exercises-for-your-herniated-disc/
Which Dr will help me in this problem (orthopaedic/neurologist/rheumatologist…etc): If you are getting surgery then an orthopaedic surgeon or neurosurgeon are helpful. However, a neurologist is not a surgeon so will give you a less biased opinion.
Will Acupuncture help to reduce back pain ? Acupuncture is most helpful most of the time.
shall I use back-belt? No, you shouldn’t use a back belt as it will weaken your back.
The above are opinions and not a recommendation. Hope that helps your disc herniation.
Sir, while putting a heavy weight on floor a sudden sound come from my back like charr and I felt pain at lower back which increases gradually day by day and it increases while doing activity like walking, sitting and bending by taking medicine pain decreases but start doing activity it comes back,my MRI findings are 1-lumbosacral transitional vertebrae with lumbarization of S1 vertebra.
2-loss of posterior concavity of L4-5 disc suggestive of early disc bulge seen.
3-mild diffuse L5-S1 inter vertebral disc bulge with propensity toward right causing mild narrowing of bilateral neural foramen (right>left) and abutting/mildly impinging bilateral L5 existing nerve roots more on right side.sir please tell me is it serious and about do’s and don’ts.
Author
Thanks for your question Shalidenra. The problem is you were born with a “transitional vertebrae with lumbarization of S1 vertebra” You normally have 5 vertebrae that are fused to form a sacrum. In your case, the S1 vertebrae did not fuse. In other words, you have an extra vertebra. This causes changes in your biomechanics so, this will require help from a professional that can examine you and take a proper history.
Does it look serious? It doesn’t look too serious if you look at the disc. However, you have the complication of lumbarization which has the potential to slow progress.
Do’s and don’ts? I can only tell you what people generally benefit from. Due to the changed mechanics of your spine the generalities may not apply to you. For example, it is best not to forward bend often or sit for long periods of time without getting up. Generally you should bend do extensions or cobra exercises. For the most part, you should do the exercises that I have here in this article.
Hope that helps your disc herniation.
Sir My self Dileep. G age of 20 years male. I have a problem means a lot of pain while speed walking and slow running also and suddenly collapsed and it occurs from above 5 months after that I went to a orthopaedic and I have scaned and in knee there is no problem after that I went to a Neurologist there I taken a MRI LUMBAR SPINE that gives a result of ” Mild disc bulges at L3-L4, L4-L5 With adequate Spinal canal and neural foramen”.
Sir I have a pain at lower back and entire left leg and a small pain at right leg.I took a medicine for a past 15 days and there is no complete relief. It gives a few hours relief and pain comes back. Please give me a suitable suggestions. In a mean while a, have a small pain at hands also. Please give me suggestions sir.
In 2013 I’m caused by a back pain and there it was a Bone TB and used a medicine for above 18 months. Sir is there any effect from that to this one. Please clarify my Doubts and give me a better suggestions.
Author
Thanks for your question Dileep. Try these exercises here: https://www.bodiempowerment.com/herniated-disc-part-2-the-best-exercises-for-your-herniated-disc/
The above is an opinion, not a recommendation. Hope that helps your disc herniation.
Sir
my mother suddenly lost control over her legs ,like when we touch her feet she can feel but her they become numb and she also lost control over her bowel ,in the MRI we found
there is mild disc bulge at d10-d11 level with presence of a extra medullary epidural / intradural lesion of approx size 12.7 x 8.3 mm noted anteriorly causing sever compression over the spinal cord and resulting in canal stenosis .
mild disc bulge at l2-3 and l4-5 level .
we went for surgery after 8 days ,surgery of decompression was done.
but still the condition of legs is same ,and no bowel sense .doctor told us it will take 3-4 weeks as you
come very late for the surgery .
i m little worried ,can you please tell why it is taking time and is it normal .
Author
Thanks for your question Sunil. There is usually inflammation as the area has to heal right after surgery. For some people, they feel relief right after surgery. I hope that your mother recovers fully. There is a chance that some or all of the symptoms may remain due to the pressure causing damage to the spinal cord. The best person to ask is the surgeon who will know the most when you go for a follow-up. I hope that things work out.
The above is an opinion and not a recommendation. Just a chiropractor in downtown Toronto.
Hello Dr.ken
I did my MRI a week ago.
where finding:
vertebra- normal
no canal stenosis or foraminal narrowing is seen
visualized cord and conus appear normal
paravertebral soft tissue appear normal
But impression is ;
At L5-S1 level:broad based posterior disc herniation causing thecal sac indentation.
Please advise me what should I do In this stage.
Author
Thanks for your question Imran. I cannot help you unless you write in detail about your symptoms. Your MRI may or may not be relevant to your case. 30% of 30 year old with no pain have disc herniations. Why don’t they have pain? Similarly, your disc herniation on MRI doesn’t mean that is the cause.
Hope this isn’t a case of diagnosis by MRI.
Hi Dr. Ken,
Myself Riyaz, I am 51 yrs old, male, have mild pain at lower back and to the right side of my waist whenever i bend, my MRI result is as follows: “Cervical, dorsal and lumbar spondylosis changes. Straightening of cervical spine – suggestive of paraspinal muscle spasm.
C5-C6 and C6-C7 intervertebral discs show diffuse bulge causing compression over thecal sac without neural compression.
D9-D10 intervertebral disc shows mild diffuse bulge causing indentation over thecal sac without neural compression. no evidence of cor compression or cord lesion.”
Kindly advice what shd be my exercises to come out of this pain.
Thanks,
Author
Riyaz: The question is whenever you bend your neck? lower back? midback?. You need to write a lot more detail before I can answer you.
Hello Doctor, My MRI of Lumbosacral Spine revealed:
1) Mild diffuse bulge with right paracentral protrusion of the L4 L5 disc indenting the thecal sac and impinging on the right traversing nerve root.
2) Mild posterior bulges of the D12-L1 and L2-L3 disc indenting the thecal sac without significant neural compression.
I was advised a few excersises which is not really helping. There occurs a pain in the right side of the waist and travels to the buttocks at times if I run or play some sports. I am really confused and dont know what should be the right treatment for this. Your kind advice will be very helpful and highly appreciated.
Author
Thanks for your question Rajesh. You need to give a lot more details of your symptoms and not just one line.
Hello Sir..I am S Thapa..34 yrs..I am having lower back pain from past couple of months and I am moving for a course of 6 months which include hectic physical activities including horse riding..
I am not able to do physical activities like running and all..Whenever I do my physical activities the pain starts…The pain is like a continuous pinching session in lower back.. The pain use to increase in both side of lower back as I use to exert more…
Recently I have done my MRI done and the report is Subtle disc bulge at L 4-5 level intending the thecal sac… Sir I request you to kindly advise me should I go ahead for the course normally or should I do with some physical excuses or which medicine I should continue… Regards…
Author
Thanks for your opinion S Thapa. Not sure what you mean by “go-ahead for the course normally” I think you are trying to say should I do my normal activities. You should do your walking by I wouldn’t do weights or horse riding. Lifting heavy objects and repeated bending of at the waist, like toe touches are not recommended. As for medication, I cannot recommend any as that is out of my scope as I cam a doctor of chiropractic.
Hope that helps your disc bulge. The above is an opinion and not a recommendation.
Dear Doctor,
My wife is feeling pain in the hip area and down on one leg. this pain started about 7 months ago, and this could have been caused by a midwife during delivery. The MRI scan impression reads: ” L4-L5: Circumferential posterior disc bulge is causing anterior thecal sac indentation with impingement of exiting nerves on both sides.
your expert advice would be appreciated.
Author
Thanks for your question Abdikadir. Can you explain why you think the midwife caused the disc herniation? I have never heard of anyone having a disc herniation during delivery. Most births don’t involve getting into positions that would cause a disc herniation. Also, most disc herniations happen over time and you feel it when you do something but the disc was already damaged before the incident. For example, you go to lift something off the floor. The lifting only pushed the disc out further but most of the damage had occurred previously as †here are no nerves in the inner 2/3 of the disc. Only the outer 1/3 has nerves so you don’t feel the damage at all. That’s the reality.
Just so you know, it is quite normal to have those exact finding in people that sit all day or people that have do manual labour with no trauma whatsoever. It doesn’t necessarily mean that the problem is a disc herniation. Your wife can do these exercises, provided the problem is a disc. https://www.bodiempowerment.com/herniated-disc-part-2-the-best-exercises-for-your-herniated-disc/
If the problem is not a disc the exercises will not help. The above is an opinion and not a recommendation.
Hope that helps your herniated disc. If you have any more questions for this Toronto downtown chiropractor I will do my absolute best to give you a great opinion.
Hi,
Please I need an explanation for this ct-scan result
“multilevel inferior lumbar degenerative disc bulges compressing the thecal sac and both nerve roots at L4-L5 level”
Author
Thanks for your question Hashim. First, your symptoms and your CT often don’t correlate, meaning your CT finding may have nothing to do with your pain or other symptoms. Remember you are trying to fix your symptoms and not the MRI. If you want to fix your MRI you will never finish. The key is your history and exam. Your CT is secondary and not as important unless getting surgery.
Your CT says that you have pinched nerves due to bulging discs.
Hope that helps your disc herniation. If you have any more questions for this chiropractor downtown Toronto, I will do my best to answer your questions.
I, Madhu taneja , 60 yrs, having severe pain for last 5 days in my right leg from the back side of hip to down the tow. MRI L/S done. there is straighting of lumbar lordosis. mild degeneraTIVE CHANGES ARE SEEN IN L/S WITH SMALL MARGINAL OSTEOPHYTES AT MULIPLE LEVELS.. iNTERVERTEBRAL DISC SHOWN DEGENERATION AT L4-L5 AS EVIDENCED BY THE LOSS OF BRIGHT SIGNAL OF NUCLEUSW PULPOSUS ON T2W IMAGES. . AT L5-S1, TNHERE IS DIFFUSE DISC BULGE CAUSING INDENTATION OVER ANTERIOR THECAL SAC.. aT L4-L5 THERE IS DIFFUSE DISC BULGE WITH RIGHT PROPENSITY WITH MILD LIGAMENTUM FLAVYM HYPERTROPHY CAUSING INDENTATION OVER ANTERIOR THECAL SAC AND NARROWING OF BILA.TERAL LATERAL RECESSES AND NEURAL FORAMINA(RIGHT>LEFT) WITH INDENTASTION OVER BILATERAL DESECENDING NERVE ROOTS. PLEASE SUGGEST AND OBLIGE. THANKS
Author
Thanks for your question Madhu. Please give me a detailed history of your problem of what makes you worse, positions, activities, how it happened. MRIs are of limited use without a proper history and exam.
Thanks for understanding that there is a lot more to back pain than an MRI.
HI my self Aradhya i am having pain in above neck region and left hand also. after MIR scan it was concluded that posterior bulge of L4-5 disc indenting the thecal sac and impinging on bilateral exiting and traversing L4 & L5 nerve roots respectively with spinal canal stenosis.
please could please suggest us what needs to be done. whether any major problem is there?
Author
Thanks for your question Aradya. I cannot suggest anything at this time as you are talking about two different things. You are talking about an MRI of your lower back and neck and hand pain. You are not giving me the proper information. Also, there isn’t enough detail on your symptoms.
Hope you understand you have give me a detailed narrative of your problem. If you include MRI results they have to correlate to the area of the body that is in pain.
Hii.
I am N .patil from mumbai & 29 years old…..im having pain in right leg ( standing and walking time )..
After MRI we found L4-L5 disc reveals diffuse posterior bulge indenting on anterior thecal sec causing narrowing of bilateral neural foramina abutting exiting nerve roots,
Doctor says start a physiotherapy for one month.. I would like to know how much time to take for full cure ..
Author
You have to give me a lot more details about your symptoms about aggravating factors, relieving factors etc.. You need to write at least a paragraph about your pains, not your MRI. Many times your MRI is not relevant to your pain. Symptoms are the key.
Hello I am Mahesh from Bangalore and I’m 22 old…
Im hvng vry bad pain n my backbone and afrt MRI we found dis “L5-S1 disc annular bulge with superadded broad based centric herniation/ caudal extrusion causing thecall and bilateral S1 neural compromises” I would like to know how will I get it cured?
Author
Thanks for your question Maheshwaran. You will have to give me much more detail on your symptoms. Your MRI results are the least important compared to symptoms. So be detailed.
Hi My Name Is Lalo I Had Surgery For A Herniated Disk In May 2017 Had It For 10 Month’s Before Surgery It Has Been 5 Month’s Alreadyg Still Have Back Pain,3 Of My Toe’s On My Left Foot Stayed Completely Numb Also A Part Of My Foot Even When I Go To The Restroom Number 1I Feel It On My Toe’s. The Measurements Of The Disc Was 5×9 By 9×9 AP Transverse. I Requested Another MRI Done It 2 Week’s Ago It Say Disc Level’s L5 S1 Increasing Size Of Left Paramedian Posterior Disc Herniation With Mild Extrusion Disc Measures 6mm Diameter By 8mm In Transverse Dimension Deflection Of Emerging Left S1 Nerve Also Mild Scar Through Surgical Port Along Thecal Sac What Does This Mean.
Author
Thanks for your question Lalo. Your MRI means that you still have a disc herniation after the surgery with some scar tissue. It would be prudent to get some professional help and get some flossing and rehab of your lower back done.
https://www.bodiempowerment.com/sciatica-4-best-exercises/
Keep in mind these exercises can make you worse so you must do them with supervision. You should not attempt to do them on your own.
Hope that helps your herniated disc.