Managing Disc Bulge: Effective Strategies for Pain Relief

Do you have a disc bulge that is causing you incredible pain in your lower back?
Does your disc bulge give you sciatica or pain down your leg?
Have you wondered what’s going on in your lower back to cause all this pain?
In this issue of Bodi Empowerment, I go over what’s going on with your disc bulge, the cause of your pain and what kind of treatments are best for you. In other words, I act as a guide to help you decide what to do.
Disc herniations, or disc bulges occur when the disc that is found between vertebrae in the spine is damaged. Most of the time the damage occurs in stages.
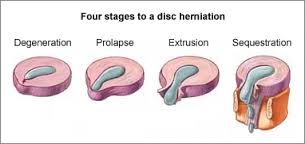
Here are the four stages of a disc herniation or disc bulge:
- Disc Bulge
- Disc Prolapse
- Disc Extrusion
- Disc Sequestration
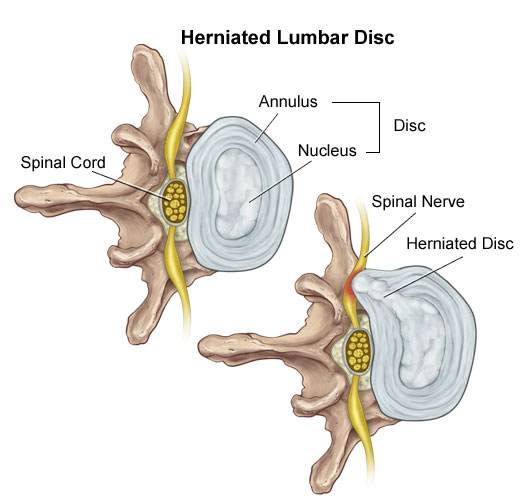
Think of the disc as a flat hard onion with strawberry jelly inside. The jelly is the nucleus while the onion layers form circular layers of hard cartilage called the annulus.
Disc Bulge
If you were to damage the annulus (onion) enough the disc gets to a point that when you bend forward, you pinch the front of the onion so it starts to bulge the onion at the back by pushing the nucleus (jelly) backwards.
This is called a disc bulge. For most of you, there is no pain but for some of you, there can be considerable lower back pain and even sciatica from this small disc bulge.
Disc Protrusion
A disc protrusion is like a disc bulge that comes out even more in one focused spot. The disc pushes out as if you had your finger inside a balloon and pushed out.
Most of the layers of the onion (annulus) have been damaged but the jelly (nucleus) is under considerable pressure. The jelly (nucleus) squeezes through the layers of the annulus (onion) with the few intact layers of the onion (annulus) and the PLL (posterior longitudinal ligament) holding the jelly from spilling out. The disc is still contained by the annulus and PLL ligament. ie the balloon hasn’t popped.
Disc Protrusions usually cause quite a bit of lower back pain and often times sciatica. Many of you, with disc protrusions, on the other hand, have absolutely no pain. There is no clear reason. A study found that 40% of people with no pain whatsoever had disc protrusion confirmed by MRI (Magnetic Resonance Imaging Machine) [1]
The trick is not to let your doctor diagnose you based on just an MRI. An MRI that shows a disc protrusion by itself is not a diagnosis. It’s what a normal person with no pain can have. Make sure there is other evidence!
Disc Extrusion
Disc Extrusion is a disc bulge so large that it breaks through the last layers of the onion (annulus) and the PLL ligament pushing into the area of the spinal cord. ie. The balloon has popped. If you have an extrusion you likely have a tremendous amount of pain leg pain and usually some lower back pain.
Surprisingly when a group of normal people with no pain were scanned with an MRI 18% were found to have disc extrusions (severe disc herniations). [1]
When you have a disc extrusion chances are the extrusion is likely causing your pain as it’s so large.
Disc Sequestration
Disc sequestration occurs when a piece of your jelly (nucleus) that breaks through the onion (annulus) and the PLL ligament has now broken off and moved away further into the spinal cord area. When you have a disc sequestration you have a tremendous amount of leg pain and some lower back pain.
Smaller Is Better: Disc Bulge
Disc Herniations or slipped discs are better if they are smaller, right? You will have less pain right? Yes except when they give you pain. Remember all those normal people with no pain with all kinds of slipped discs? They had disc bulges, disc protrusions, and disc extrusions and even disc sequestrations with no pain.
On the other hand, even with a small disc bulge, you can get a lot of pain and even sciatica with no pressure on the nerve. So smaller isn’t always better.
Bigger Is Better: Disc Bulge
Sometimes bigger is better. Most people like you with disc extrusion and sequestration have lots of pain. The fact is these painful extrusions while more painful usually shrink with time. It takes about a year but with the shrinking of the herniations, the pain does decrease.[2-5]
Disc Herniation: Disc Bulge Treatment
#1 Stop Aggravating Yourself
Half the problem why people don’t get better is that they continually aggravate their lower back and their slipped discs. Learning to lift properly, sit properly and even stand over the sink while brushing your teeth properly can help you avoid the pain.
Even Yoga exercises such as the downward dog can aggravate the lower back, Pilates and even your basic abdominal crunch have been shown by Dr Stuart McGill to increase the pressure in the disc beyond its safe limit.
If you want to find out how to stop aggravating your lower back, click the link below.
See Also: Slipped Discs: Best Self-Treatments To Help Your Lumbar Disc Herniation
#2 Exercise For Disc Herniations / Slipped Discs
For complete instructions on exercises for slipped discs click the link. Best Exercises For Your Slipped Disc
#3 Chiropractic Adjustments For Disc Bulge
A major research paper showed that people who have had lumbar disc herniations who have failed at least 3 months of medical management, including treatment with analgesics, lifestyle modification, physiotherapy, massage therapy, and/or acupuncture, should consider chiropractic spinal manipulative treatment, followed by surgery if unsuccessful. [6]
I would also add that I would try 3 different chiropractors as the competency level varies from person to person. Like any profession including medical doctors and physiotherapists, there are the good ones and bad ones.
See also: 6 Things You Should Look For In A Chiropractic Clinic
#4 Acupuncture For Disc Bulge
Acupuncture is helpful for Slipped Discs in the neck and the lower back.[7-8]
#5 Injections
In a study of two different groups getting treatment for lumbar disc herniations, the group getting chiropractic manipulation had 76.5% of the people improve while the group getting the nerve root injections improved by 62.7%.
After a month, the chiropractic spinal manipulation group had a 60% reduction in pain compared to the nerve root injection group, which had a 53% decrease in pain. Keep in mind the nerve root injection group seemed to be worse to start with compared to the spinal manipulation group.
See Also: Chiropractic Spinal Manipulation Vs. Nerve Root Injections for Lumbar Disc Herniations
Epidural injections are also helpful for lower back pain and the radiating pain down your leg.[8]
#6 Surgery
#1 Discectomy
There are two types of surgery available for slipped discs. Discectomy and spinal fusion. This surgery involves cutting out the piece of the disc that is protruding out and pushing on the spinal cord or nerve.
Discectomy is relatively simple compared to spinal fusion. You have a much better chance of success with discectomy if your MRI shows that your disc herniation is greater than 7 mm thick and correlates well with your neurological exam and nerve conduction studies.[9] If your lower back pain is greater than your leg pain discectomy will not likely work very well for you.[10]
#2 Spinal Fusion
Spinal Fusion removes the disc herniation, jelly (nucleus), and most of the annulus (onion). Bone from the pelvis is then transplanted where your disc was so that the two vertebrae become one.
What Treatment Should You Do?
You should do at least 3 months of therapy when you have a slipped disc before even considering surgery or injections. Start by not aggravating your lumbar disc. You need to modify how you bend forward, lift and even pick up your socks.
See Also: Disc Herniation: Best Self-Treatments To Help Your Lumbar Disc Herniation
If you have trouble sleeping at night you can take painkillers to help you get a better sleep. Don’t stay in bed though. When you have excruciating pain you should only have bed rest for a maximum of two days total.
Next, try chiropractic or physiotherapy with someone who also does acupuncture. Make sure it’s not with somebody who knows how to do 20 acupuncture points. Be patient with them as disc herniations can be difficult to deal with.
Attend regularly 3 times a week for at least a month. Make sure they change the treatments to find what works best for you. If they keep doing the same thing each visit but you are improving that is fine, but if you aren’t improving then it’s time to find a new chiropractor.
If you don’t get any better after a month change to a different chiropractor. I recommend trying 3 different chiropractors as different chiropractors have different training.
If you plateaued or haven’t improved at all then it’s time to get a nerve root injection or an epidural injection. Make sure it’s with a person that does this every day. An emergency room doctor or family physician only does this procedure once in a while. It’s better to get someone more experienced.
When conservative care has been completely exhausted then it’s time to consider surgery. Discectomy is more conservative than spinal fusion and recovery is much quicker. You should consider discectomy surgery if you have :
- Foot drop that is getting worse.
- Any other neurological symptoms that is getting worse like your reflexes, sensitivity
- Bowel or Bladder Symptoms (loss of your poo and pee function). : This is an emergency you should go to the hospital right away.
- If you have a disc protrusion or that is 8 mm or larger that correlates well with a neurological exam, and Nerve conduction tests.
- Leg pain is worse than your lower back pain.
Beware of the surgeon who wants to operate on a small disc bulge. There are too many unnecessary surgeries in the USA especially spinal fusion.
Spinal fusion is considered when your lower back pain is worse than your leg pain
Tell us what you think in the comments below and like us on Facebook. This Toronto Downtown Chiropractor will answer all questions in the comments section.
Research
1. Weishaupt D et al. “MRI of the lumbar spine: Prevalence of intervertebral disc extrusion and sequestration, nerve root compression and plate abnormalities, and osteoarthritis of the fact joints in Asymptomatic Volunteers.” Radiology – 1998; 209:661-666
2. Maigne JY, Rime B, Delignet B. Computed tomographic follow-up of 48 cases of nonoperatively treated lumbar intervertebral disc herniation. Spine 1992; 17:1071-1074.
3. Ikeda T, et al. Pathomechanism of spontaneous regression of the herniated lumbar disc: histologic and immunohistochemical study. J Spinal Disord 1996;9:136-140.
4. Ahn SH, Ahn MW, Byun WM. Effect of transligamentous extension of lumbar disc herniations and their regression in the clinical outcome of sciatica. Spine 2000; 25:475-480.
5. Komori H, Shinomiya K, Nakai O, et al. The natural history of herniated nucleus pulposus with radiculopathy. Spine 1996; 21:225-229.
Research
6. McMorland G et al.Manipulation or microdiskectomy for sciatica? A prospective randomized clinical study. Journal of Manipulative & Physiological Therapeutics 2010; 33: 576-584.
7. Wu, Yao-chi, Jun-feng Zhang, Yi-jun Sun, Cheng-fei Huang, Ping Shao, and Gui-zhen Liu. “Clinical study on electroacupuncture for cervical intervertebral disc herniation.” Journal of Acupuncture and Tuina Science 11, no. 6 (2013): 371-374. – See more at: http://www.healthcmi.com/Acupuncture-Continuing-Education-News/1249-acupuncture-found-superior-to-drug-for-neck-disc-pain#sthash.vD0pNepM.dpuf
8. Wang HeshanNon-Surgical Therapy For Prolapse of Lumbar Intervertebral Disc. The Journal of Traditional Chinese Medicine
9. Parr AT, Diwan S, Abdi S. Lumbar interlaminar epidural injections in managing chronic low back pain and lower extremity pain: a systematic review. Pain Physician 2009;12:163-188.
Research
10. Carragee EJ, et al “Clinical outcomes after lumbar discectomy for sciatica: The effects of fragment types and annular competence” J Bone Joint Surg Am – 2003; 85(1):102-108
11. McMorland G et al.Manipulation or microdiskectomy for sciatica? A prospective randomized clinical study. Journal of Manipulative & Physiological Therapeutics 2010; 33: 576-584.
Related Categories: Acupuncture, Back Pain, Disc Herniation, Imaging, Low Back Pain, Surgery





Hi Dr Ken,
I am 46Yrs/female.
I am suffering from severe lower back pain since last 2 weeks.
Following is my MRI reports:
Bilateral paracentral protrusion of L3-L4 intervertebral disc causing indentation over ventral theca and left exiting nerve root.
Posterior bulging of L4-L5 intervertebral disc causing indentation over ventral theca.
Kindly suggest what should I do.
Author
Thanks for your question but you need to tell me more about your symptoms to give you an opinion.
Hi Dr Ken,
Thank you for your response.
In last 2 weeks, I have lower back pain and after following MRI report, doctor suggests a surgery.
Full MRI Report:
Screening of cervical spine(sagittal T2W images) show posterior bulging of C5-C6 Inter-vertebral disc without compressive elements.
Screening of dorsal spine (sagittal T2W images) appears unremarkable.
Bilateral para-central posture of L3-L4 Inter-vertebral disc causing indentation over ventral theca and left exiting nerve root.
Posterior bulging of L4-L5 inter-vertebral disc causing indentation over ventral theca.
Author
You are not understanding me. You need to tell me your symptoms. You need to be detailed. Reposting what you wrote last time is not enough to go by. Do you think your MRI report and telling your doctor you have low back pain is enough. Your doctor needs to do a thorough history and exam. You need to give me the thorough history. Like does standing make it worse, sitting etc……………………
Hope you understand that I need a lot more information than that.
Sorry for half information.
It pains when I am standing and while bending my lower back for any purpose(like picking up anything from ground while standing), it pains a lot. I am not feeling much pain while my back is straight but when I am standing for too long or bend while working it pains a lot.
And at the same time I feel numbness and tingling in my right leg.
In my house hold work, I used to lift heavy basket and climb through stairs for 2 floors daily which might cause the issue.
Author
Thanks for your comment Shobhana. You should try these exercises. https://www.bodiempowerment.com/herniated-disc-part-2-the-best-exercises-for-your-herniated-disc/
Keep in mind exercises can make you worse. You should go over the exercises with a chiropractor that knows the exercises.
Hope that helps your herniated disc. The above is an opinion and not a recommendation. If you have any more questions for this downtown Toronto chiropractor I will do my best to give you a good answer.
I am 40 yrs women, having 2 kids, few days ago i had severe back pain for which i am hospitalized,after the MRI finding doctor is saying that i have to undergo a operation, need ur advice in this regard.
I cant sit,walk or move at all.
MRI FINDINGS:
MRI lumbar spine without contrast
Multilevel sisc desiccation,facet arthropathy and ligamentum flavum hypertrophy.
Bilateral pars inreearticularis defect of L5 vertebra with mils malaligment at L5-S1 level.
At L4-L5 level, there is circumferential disc bulge with annular tear resulting in mild indentation of thecal sac and mild lateral recess narrowing on both sides.
Please provide ur opinion….should i undergo surgery?
Author
Thanks for your question Mrs Imran. It’s difficult to say whether you need surgery or not. First, I have seen many people with a pars defect (fracture of the spine with a movement of the vertebra forward AKA – spondylolisthesis) with no pain or mild pain. If you had a recent trauma or motor vehicle accident chances are what you see on MRI is related. The spondylolisthesis would then need to be treated surgically. If you didn’t have a fall or car accident the problem with your lower back may be due to the disc.
My opinion (not a recommendation) is that you should try a trial of conservative therapy such as chiropractic or physiotherapy.
Hope that helps your pars defect or your disc herniation.
My name is sukhwinder singh.
I’m suffering with backache from last 6 months.
Lots pain occurs at lower to right leg.
Can’t walk, can’t stand, can’t sit even can’t sleep properly.
MRI REPORT IS
:MR finding reveal
-Diffuse disc bulge and posterior annular tera at L3-L4 indenting the thecal sac and causing minimal bilateral neural canal compromise.
-Diffuse disc bulge and right paracentral disc protrusion with caudal migration at L4-5 causing spinal canal stenosis with bilateral neural canal compromise (R>L) and impinging upon the right traversing nerve root.
Author
Why don’t you try lying down on your front or face down for periods of time to see if that helps? 5-10 minutes may be very helpful to get you sitting and standing.
This is an opinion and not a recommendation. If you have any questions for this downtown Toronto chiropractor I will do my best to give you a good answer.
Dear Dr. Ken,
I am a 36 years old male. I exercise often and don’t think overall my general health is bad. About 1 month ago, I woke up having pain in my neck and the top of my back. It was difficult to turn my head to one side, so I automatically assume it was torticollis which has happened in the past from sleeping in a bad position. I did what I normally did in the past, go for a massage but this time it didn’t work. I started getting pain (like an electrical feeling) going down my right arm. I went to my GP and he sent me to get an MRI done, this was the result:
The cervical curvature is reverse (kyphotic). No evidence of listhesis. No evidence of compression fracture in the vertebral bodies. There is decrease in the signal intensity of the intervertebral disc at C5-C6 & C6-C7 level with associated thinning of the intervertebral space height and mild posterior central of its discs causing irritation of the thecal sac. Spinal cord with lateral root nerves and CSF show no abnormality. No tumor is noted. Lateral masses and other posterior elements are also normal.
Impression:
Reverse cervical curvature. Disc desiccation with degeneration and bulging causing irritation of the Thecal Sac.
Unfortunately, where I live I don’t have access to a chiropractor. I have downloaded the Egoscue video exercise program but it seems that their exercises focus more on the hips and core and I’m sure is great for posture and to avoid future pain in other areas, etc… I also just read the 7 steps to pain free life (The Mackenzie Method) this exercises seem to help but it is painful when I perform some of them and I’m not sure if I should stop or go through with the pain as it will go away eventually.
I’m really frustrated because part of my work is sitting behind a computer which right now it proves to be difficult to do and I love training (specially weight lifting) but I’m afraid to get in the gym as I’m not sure if it will make it worst or it will help. The pain just seems to be there and get worst when I’m in certain positions and it seems to feel better when standing or laying down.
For what I have read so far and the information that I have found, the problem with the cervical curvature should be able to be corrected with exercises, posture correction etc… (Please correct me if I’m wrong) My main problem right now is the disc desiccation with degeneration and bulging causing irritation of the Thecal Sac. For some reason, I seem to find much more information for problems in the lumbar and mid spine then in the cervical region.
Could you please be so kind to let me know whether my problem has a solution? what would you advise me to do? Any specific exercise maybe? Maybe you can advise of another program that suits my problem better than Egoscue and Mackenzie? Please help…thank you.
Author
Thanks for your question Jonas. I would do the exercises here in this article.
https://www.bodiempowerment.com/cervical-disc-herniation-best-exercises-help-sore-neck/
However, I would do the both exercise lying down and not be sitting up. I would also be gentle. These exercises really should be shown to you in person by someone local as any exercise especially in your case can make you worse.
That’s my opinion anyways. Hope that help your cervical disc herniation. If you have any more questions for this downtown Toronto chiropractor, I will do my best to give you helpful answer.
Hi there. I am a 29 year old female and I was in a car accident a year ago. I did not have an MRI immediately after but felt a lot of pain for a few weeks. I recovered and when I traveled by plan in December, I developed an intense pain in my low back and sacrum – felt a lot like sciatica. I was diagnosed with a disc bulge in my L5-S1 via CT. I was already in chiropractic care and so he ordered an MRI. MRI showed L5-S1 left subarticular disc protrusion impinges on the left S1 nerve root entering the left lateral recess. Since December, I’ve been in chiropractic care, physical therapy, yoga, pranic healing, have received massage, two injection in L5 and S1 and nothing have offered relief. My pain is most intense in my left sacrum area – left buttocks and runs down the leg, like a pulling feeling. My left leg and foot often tingle or feel numb. Strength is still pretty good. I had increased pain after injections. The pain is constant and worst when I sit. It feels I am sitting on a pole. I saw a neurosurgeon who is suggesting a left sided L5-S1 medial facctectomy, hemilaminotomy with possible microdiscectomy. I am seriously considering it as I really want to get my quality of life back and at least take the edge off of this nerve pain in my buttocks and leg. Any thoughts of suggestions?
Author
Thanks for your question Erin. Sounds like you have a lot of pain. You can try these exercises https://www.bodiempowerment.com/herniated-disc-part-2-the-best-exercises-for-your-herniated-disc/
concentrating on the cobra exercises. However, the exercises are not customised to you so they may aggravate you. You need someone in your city or town that can help you customise the exercises. I would say try another chiropractor or another physiotherapist that has a great reputation. While not guaranteed, they are more likely to be able to help.
This is an opinion and not a recommendation. If you have any more questions for this downtown Toronto chiropractor I will try my best give you helpful recommendations.
Hope that helps your slipped disc.
Thank you!
Author
You are welcome.
Sir, My mother suffers from lower back pain from the last 12 years, she had numbness in bothe legs, tingling in left leg, uncontrolable urine flow, pain increases when climate change to cold, or when overworks.
Last month she undergone for a MRI test, here are the impressions:
MR imaging reveals degenerative changes with:
1.Subtle small left central bulge of L2-L3 disc indenting the thecal sac.
2.Mild posterior annular bulge of L4-L5 disc with bilateral ligamentum flavum
thickening (L>R) causing narrowing of bilateral lateral reces?
Author
Thanks for your question Dipinder. Your mother is too far gone for me to help. She needs to have an immediate consultation with another doctor to get another opinion to see if this is cauda equina syndrome.
Good luck with your mother’s condition.
Sir: I had lower backache 4-5 years back after i lifted something heavy. Got cured by a month of Physiotherapy. The only problem I’ve had is backache after long period of standing up – which got cured after a good night sleep.
Now since the last 6 months I have symptoms of numb right feet ( feeling of heat radiating from sole and of ants crawling) and in left feet or sole to be more exact of occasional cramping ( feeling as if someone pulled a string halfway between the sole. Numbness feeling in right sole is very prominent and constant. Left sole pain is occasional- maybe once in few days. Backache also returned since last 2 weeks. I did MRI yesterday and here are the findings. Can you please suggest the treatment. I do not tolerate a lot of medicine well.
++++++++++++++++++++++++++++++++++++++++++++++++++++++
FINDINGS:
Transitional vertebra is seen at lumbo sacral junction with sacralisation of L5. Lumbar lordosis is
straightened. Mild retrolisthesis of L4 over L5 and of L2 over L3 noted.
Tiny hemangioma noted at L3, L5. Marginal osteophytes are noted at multiple levels.
Vertebral bodies are normal in height , outline, marrow signal intensity and alignment. No osseous
destruction seen. Facet joints are normal. Bony spinal canal at vertebral bodies level is normal in
dimensions.
Dessicated discs are noted at multiple levels at D12-L1, L2-L3, L3-L4 and L4-L5.
Diffuse disc bulge is noted at L4-L5 along with bilateral ligamentum flavum hypertrophy, annular
tear on left side causes indentation over thecal sac with minimal bilateral lateral recess
compromise. Loss of fat plane is noted around exiting nerve root suggest possible compression.
Mild disc bulge is seen at L5-S1.
Indentation over thecal sac is noted at D12-L1 ,L1-L2, L2-L3.
Thecal sac is adequately capacious.Fat plane around exiting nerve roots is maintained at all levels.
Lower dorsal cord is normal with no evidence of focal or diffuse signal abnormality.Cord-CSF
interface is well-marginated.
Both sacroiliac joints are normal.
Pre-vertebral and para-vertebral soft tissues are normal.
Tiny cyst is noted at left kidney lower pole.
OPINION:
Lumbar spondylosis with degenrative disc disease at multiple levels as described above , more
at L4-L5 with possible compression of left exiting nerve root.
Author
Thanks for your question Rajbir. Looks like your disc has herniated again however the MRI doesn’t exactly correlate. This can be related to the fact that the MRI is taken lying down while your symptoms likely get worse with sitting and bending along with what you mentioned standing for long periods. What I am saying is the MRI doesn’t show what’s going when you doing other things other than lying down. The MRI shows the disc to be out to the left when lying down but the disc can change positions when sitting up. You should go back to your physiotherapist.
Hope that helps your slipped disc. If you have any other questions this downtown Toronto chiropractor will do his best to give you a sound opinion.
Hello Dr,
My Daily routine consists of 3 hours of cat travel and 9 hours of office work (mostly sitting on a computer).
I do weight lifting for 3 days a week ( 1 and half hours daily). I have started weight lifting in August 2016.
On january 19th, i got pain on my right leg (From buttock till knee). No foot numbness.
I stopped doing excercise and went home.
Next day the pain was localized to right side buttock.
For next 10 days it remained the same.
On 29th January, while going for a outing i drove the car for 4 hours. During that i got very severe pain like electric current on my right leg ( buttocks till knee). The shock was coming at a particular sitting position only. Also there was no numbness. Some how i put my GYM back belt and drove back.
Since then i never got the shock pain.
But next day i did my MRI with 1.5 Tesla.
The report says as below.
Mild diffuse posterior bulges of L4-L5 and L5-S1 discs indenting the thecal sac without significant neural compression.
Screening of Cervico-Dorsal Spine is unremarkable except for reversal of cervical lordosis.
Lumbarization of S1 Vertrebra. Normal curvature of spine is maintained.
Dr. advised to do complete bed rest for one week with day phisiotherapy.
I did the phisiotherapy and did bed rest for two weeks.
Intermediate rest for third week.
During the second and third week i did the back excersice daily.
Now the pain is not there. Plus i stopped driving.
This week i have started to go to office.
Please let me know if the MRI report says anything serious.
Regards,
Mahesh
Author
Thanks for your question Mahesh. Sounds like you are a lot better now. To answer your question the MRI does show a disc bulge but if you take care of yourself by getting a lumbar support roll while sitting and having good posture and doing the exercises that should be enough to prevent most but not all future incidents. If they do reoccur you should be able to take care of the lower back disc herniation quite quickly.
Hope that helps your disc herniation.
Hello Dr Ken,
Here is the impression of my spouse MRI taken in Sep 2013.
MRI of lumbo-sacral spine reveals diffuse disc bulges at L3-L4, L4-L5 & L5-SI levels causing mild thecal sac indentation and attenuation of bilateral neural canals Mild extraforaminal indentation of the exiting L5 nerve root on left side is visualized.
After that she started her physio and exercise for few months and got some relief and then STOPPED doing it and gave gap. Now from last one month the pain came again and this time it makes her left leg numb. she is now on pain killer and anti inflammatory drugs so that she can continue her exercise and physio. we are waiting for her latest MRI to be don now.
I just want to know from your expert advise that does she require any epidural injections or surgery at this stage? Or she should continue having anti inflammatory meds and pain killers and keep on doing her physio and exercise to avoid injection and surgery?
Author
Thanks for your question Ripu. Sounds like she needs to go back to physiotherapy for a while again.
Hope that helps your spouse’s slipped disc.
Sir i m mr Shiv Chand
Age 34
I m getting problem in lower back.
Plz give me some ex tips.
I have done MRI and report is…
Posterior diffuse disc bulg with mild compression over right exiting nerve roots at L4 L5 interverteral disc level.
Author
Thanks for your question Shiv. I can’t give you any opinion. You need to write a lot more detail probably 10 times what you wrote. Not the MRI just your symptoms.
Hope you understand it’s a lot more complicated making an opinion on slipped discs.
Hello Sir,
My Aunt is suffering from,
# POSTEROCENTRAL AND RIGHT POSTEROLATERAL HERNIATION OF L-5/S-1 INTERVERTEBRAL DISC LEADING TO SMOOTH INDENTATION OVER THECAL SAC WITH BILATERAL NEURAL FORAMINAL STENOSIS
# DEGENERATIVE CHANGES IN LUMBAR SPINE.
We are no sure whether go with surgery or not.
Please help.
Author
Thanks for your question Kapil. If you read the hundreds of posts I cannot comment on a simple MRI. Lots of people have a lot worse with no symptoms. In other words, the MRI by itself is not enough. Also always do conservative therapy first.
Hope that helps your slipped disc.
Hi Dr. Ken,
I’m 24 years old male and it’s been around 6 months i’m suffering from lower back pain. I recently got my MRI done and it says the following:
1. posterocentral protrusion at L5-S1 indicating the anterior thecal sac without any neural compromise
2. The lumbar curvature is straightened with normal alignment likely muscular spasm
3. L4-5 disc shows loss of posterior concavity, abutting the thecal sac. Bilateral neural foramina are normal
4. All IVDs are normal in height and signal intensity
5. Rest of the IVDs shows no protrusion/bulge. Thecal sac and bilateral neural foramina are normal
Can you please explain this is leighman terms and what needa to be done in order to get rid of this problem and what are the chances to get rid of such a problem. Your inputs would be highly appreciated
Author
Thanks for your question Punit. You only told me about your MRI. Diagnosis are made by history and exam, not an MRI. You need to tell me a detailed history and exam before I can comment. If it’s not detailed enough than I cannot even give you an opinion.
Good luck with your possible disc herniation diagnosis.
Thanks for the response.
It’s been around 6 months i’m having this problem. Initially the problem started while forward bending, stiffness in back. Then I was advised by Dr.to take an X-Ray which did not shows any damage/ambiguity in the report. Then dr.advised to do some exercises like forming reverse “D” of the body(bend backwards). I did this for 2 months and now the pain also started while bending backwards. Hence, dr.advised me to take an MRI and he has now prescribed a pain killer(tramadol) and a nerve compound tablet. Just as an FYI, i do not have pain in my legs only the upper portion of buttock gives pain sensation. Please suggest, sir.
Author
Thanks for your question Punit. https://www.bodiempowerment.com/herniated-disc-part-2-the-best-exercises-for-your-herniated-disc/
You can try these exercises but it is always best to see the best local chiropractor or best physiotherapist in your area. Also don’t do the “cobra” exercise as that is the type of exercise that made you worse. You could try knee to chest exercises.
Hope that helps your slipped disc.
What happens when you have had surgery with a complete fusion from L1 to S1. I am having trouble with my legs I can’t sleep oin bed because the pain is so bad in the morning I literally can’t move without spasms one after another. They are horrible. I don’t know what to do anymore .
Author
Thanks for your question Jane. Well, if there are no complications then you feel better but you cannot bend forward much as all your lumbar vertebrae are fused together. I would personally get an injection first before considering surgery, especially surgery that drastic. I would also question why so many vertebrae need to be fused. I have never heard of such a case. Get a second opinion from someone that doesn’t stand to gain from doing the surgery.
Hope that helps your slipped disc.
I am suffering from lower back pain from last 1.5 years with the pain goes in outer side of right calf and no pain in right thice.
I am 27 year old. I am software engineer by profession from past 6 years and having continous sitting job.
While travelling in car, due to some sudden jerk i got this pain.
My MRI Report says : “The study reveals mild exaggeration of normal lordic curvature of the lumbar spine”.
And “MR finding reveals EARLY Lumbar Spondylotic and Disc Degenrative changes associated with :- Mild annular disc bulges at L4/L5 and L5/S1
level mildly indenting ventral thecal sac and bilateral descending nerve roots.”
From past 1.5 years i am doing mix of yoga, exercise, walking randomly, But did not get much relief.
Now from past 1 month i have started a fixed routine of below set of exercises :
a. Reverse corpse pose : 10 min (meditation)
b. 1 set of 5 round of Crocodile pose.: Each round of 1.5 min, then reax in reverse corpse pose between each round for 20-30 seconds.
c. Half cobra pose : 2 set of 5 rounds.
d. Snake pose : 1 set of 5 round with hand joined backside of the buttock.
e. Half locust pose : 1 set of 5 rounds for each leg, raising leg 30-45 degree.
f. Full Locust Pose : 1 set of 5 rounds.
g. Flapping fish pose : Both sides 1 by 1 with eleven deep breaths with awareness at the back.
h. Reverse Corpse pose : 5 mins (SO-HAM Meditation).
I am doing all these steps 2-3 times a day with hot water bottle at the back while doing all the poses.
Please suggest,
Should i add or remove any exercise.
Any things should i avoid and any change in diet.
Author
Thanks for your question Vinit. You asked that very same question before and the answer is still the same. That’s my opinion anyways. I would also find the best chiropractor in your neighbourhood.
Hope that helps your slipped disc.
Dear Sir,
I have been suffering with back pain for over a year now with pain on the buttock down my legs. Have been on pain killers but now the pain is unbearable on the legs n back of my thighs down to the ankle. My MRI Report says the following : Posterior midline protrusion of L4/L5 disc with associated thickening of ligaments flava bilaterally causing severe compression of the thecal sac.
Please advise if i should consider surgery. I am 53 years old.
Thanks
Author
Thanks for your question Mimi. You should try conservative therapy first. Go to the best chiropractor or physiotherapist in your city as these exercises won’t help.
Hope that helps your slipped disc.
Hi Sir
I am suffering from lower back pain from last 6 years.I am just 28 year old. While doing gym i got sudden jerk in lower back. Earlier as per MRI report it was just a minor buldge disc at l4-l5 and l5-s1.
But now a days i feel much pain at sacrum area or rectal area. I feel itching after coming from stool. Pain in knees if doing sitting more then 10 min.
During this 6 years time, I was doing yoga. but didn’t get any relief.But now that bottom part pain is unbearable.
As per latest MRI below are the points :
1)Desiccation of L5-S1 inter-vertebral discs is seen.
2)At L4-L5 disc there is a diffuse bulge with flattening of posterior concavity indenting the thecal sac and bilateral neural canals.
3)At L4-L5 disc there is a diffuse bulge indenting the thecal sac and bilateral lateral neural canals.
I have been doing Crocodile pose, Half Cobra pose,snake pose, Half locust pose, Locust Pose,Flapping pose and the following on back side i.e Leg Raise pose, Leg Lock Pose. But I feel ant eating pain near toe after doing snake pose but yoga instructor is saying keep doing yoga.
Please suggest me what i need to do further.
Author
Thanks for your question Deepak. You should not do the leg lock pose and the leg raise pose. It’s not what more you need to do but what you need to stop doing.
Hope that helps your possible disc herniation. This is an opinion and not a recommendation.
Hi Sir
Thanks for quick response.
Please let me know whether I am doing following exercise properly and in right sequence :
1)Reverse corpse pose : 10 min with slow breathing.
2)Half cobra pose : 2 set of 5 rounds.
3)Snake Pose : 5 rounds (just like cobra pose but hands joined in back side off the buttock )
4)Half Locust Pose : 5 rounds(raising legs 30 degree backside)
5)Full Locust Pose : 5 Rounds(raising 20 degree)
6)Flapping fish pose : Both the sides with 10 breathing.
Now I have stopped doing One Leg raise(alternatively) and Leg lock (alternatively).
In the last again 10 min in reverse corpse pose (meditation).
I asked with my yoga teacher about leg raise and leg lock, he said that they release compressed nerves.
Please suggest if you would like to add or remove any exercise(modification in way of doing) and changes in diet or eating something specially for back patient.
Author
Thanks for your question Deepak. The leg raise and leg lock will make most types of disc herniations worse. It does not release compressed nerve except for anterior disc herniations. Unless your Yoga teacher diagnosed an anterior disc herniation then your Yoga teacher is a medical doctor or chiropractor in which case you should listen to your Yoga teacher.
The exercises you are doing are fine at the moment. This is an opinion and not a recommendation.
Hope that helps your slipped disc or disc bulge.
Hi Doc.
Thanks for your quick responses and suggestion 🙂 . Now i would be doing these exercises for next one month and then will update my condition.
Also forgot to mention that I am doing these exercises three times in a day and keep hot bottle on back while doing all poses.
Thanks again.
Author
Thanks for your comment Deepak. The hot pack shouldn’t hurt your lower back. If the pain is persistent though, I would take the hot pack away as a first move.
Hope that helps your disc bulge or disc protrusion.
Hi Sir
I also wanted to update that I feel much pain in anus or rectal area when doing sitting more then 10min. Also feel itching pain there after coming from stool.
Am I suffering from piriformis syndrome also.
Do I need to add some more exercise for that too.
Please help me as I am not able to attend my office and suffering like hell. Is it possible to have some Skype session with you?
P.s : not able reply from our last discussion as reply link is not present there.
Author
Thanks for your question Deepak. No, you don’t have piriformis syndrome you have a yellow flag. This means that you have a disc herniation is putting too much pressure on your nerves. You should seek professional from the best chiropractor or best physiotherapist in your area.
Hope that helps your slipped disc.
Hi Doc
As you suggested me to visit some physiotherapist, I had visited one.
They asked me to do following things:
– walk for some distance.
– pressed my back with hands and for pain area but i didn’t feel any pain while if it is pressed.
-move forward after which i felt pain in calf and back.
-checked my whole bare back
I told them that i feel pain near anus, perineum and at knees when i sit more then 10 min
They said my body is structurally OK and after looking at MRI he said it is normal but they finally made conclusion that my pelvic is tilt. He show me some pelvic crossed syndrome pics on google.
Then during physiotherapy session he made me some stretching like legs raise, hips bent. pressed hardly using hands on my left and right side of abdomen. He suggested me to apply ice pad for some days near anus. He suggested me not to do any exercise for some days and used donut cushion for sitting.
Author
Thanks for your comment Deepak. Hope your slipped disc gets better with your physiotherapist.
My is 42 yrs old, for 1 month he has been suffering from back pain and leg pain. In his MRI results were 4-5 paracentral disc herniation . What do u think is the best treatment a surgery or by medicine or therapy???
Ap diameter of spinal cana at l5s1l is 7 mm .
Occasionally pain radiates down .
Is it a case of surgery?
Hello Dr. Ken.
I am 32yrs/Male. I am an instrumentation engineer and long travelling, lifting heavy objects and standing/sitting in improper postures for long times is part of the job. I have a lower back pain that moves towards the legs. It started around two years back when i was working on an installation. The pain usually starts when i lift heavy objects or sit/stand for a longer time the epi center of the pain is lower back right side and if i continue working in the same way the next day the pain starts to go down from my lower back towards the knee. When the pain is extreme i often feels pinching pain when ever i make a move. Then with proper rest, pain killers, physiotherapy, analgesic creams the pain reduces and fades away till i again aggravate my body.
In order to go in to the depth of the issue i consulted an orthopedic and spinal surgeon who recommended MRI to study along with my history. Below is the MRI findings:
Normal Lumbar Iordotic curvature seen.
At D11/D12 level there is a disc dessication and degeneration with superimposed disc bulge shows central and right paracentral disc protrusion along with ligamentum flavum hypertrophy causing thecal indentation, right neural foraminal narrowing with radicular compression as well mild indentaion over the right sided cord.
At L5/S1 level there is a circumferential disc bulge with central and right paracentral disc protrusion causing central canal stenosis and bilateral lateral recesses narrwowing with nerve root impingement more on the right side.
Rest of the intervertebral disc spaces appears unremarkable.
Distal spinal cord appears normal.
Doctor asked me the pain intensity and asked if i think i can manage the pain he will not go for surgery but if the pain is unbearable then the surgery is the only option. My pain is right now manageable with meds, body relaxing and physiotherapy. He has advised me to reduce weight, dont lift heavy objects and dont sit or stand for longer periods with bad posture and go for physiotherapy as and when required.
I want to know what do you think?
What are the exercises that i can perform at home to reduce pain?
What are the other things i should avoid?
Thanks and Regards
Farhan Khan
Author
Thanks for your great explanation and your questions Farhan. Sounds like your surgeon is being reasonable and trying physiotherapy first before exercises. I’m not hearing a lot of reasonable or sound judgement in my opinion from a lot of others so this is refreshing.
You can do these exercises but you can get worse as I haven’t got your full history and haven’t examined you. You know you are getting worse if the pain or other symptoms go further down the leg.
https://www.bodiempowerment.com/herniated-disc-part-2-the-best-exercises-for-your-herniated-disc/
You should have these exercises supervised by a health practitioner.
Avoid bad posture. This is a opinion and not a recommendation.
Hope that helps your herniated disc.
Hi Dr. Ken,
I had previous back surgery and about 5 or 6 years ago. Everything has been ok but over the past 2 months I have had low back pain mainly on the left side. I get the worst pain when I sit up. I had an MRI yesterday and Will post the results bellow. My follow-up is over a month away . Not sure if I should try to get in sooner or what to do.
EXAM DATE AND TIME: 12/05/2016 10:08 AM
MRI LUMBAR SPINE WO/ WITH GAD
TECHNIQUE: Sagittal T1, T2, and STIR; axial T1 and T2; post gadolinium sagittal and axial
T1-weighted pulse sequences of the lumbar spine were performed. 15 mL MultiHance
gadolinium was administered intravenously.
PRIOR EXAMS: Relation is made with MRI lumbar spine dated 10/17/2014.
FINDINGS
VERTEBRAL HEIGHT: The vertebral bodies maintain normal height without compression
deformity. Postoperative changes are seen from posterior lumbar fusion at L5-S1 with
pedicle screws and posterior stabilization rods.
VERTEBRAL ALIGNMENT: There is normal alignment without spondylolisthesis.
VERTEBRAL BONE MARROW: There is no evidence for marrow replacement.
DISC SPACE: Intradiscal fusion at L5-S1. Decreased disc height and signal within the L3-4
and L4-5 intervertebral discs is consistent with disc desiccation.
PARAVERTEBRAL SOFT TISSUES: Unremarkable.
LEVELS
L1-L2: Unremarkable.
L2-L3: Unremarkable.
L3-L4: Mild posterior disc bulge flattens the ventral thecal sac. There is no significant
stenosis.
L4-L5: Mild posterior disc bulge flattens the ventral thecal sac. Hypertrophic changes of
the posterior facets are seen. There is no significant stenosis.
L5-S1: Postoperative changes are seen from posterior lumbar fusion. Right paracentral
enhancing epidural scar is again noted. There is no significant stenosis.
CONUS: The conus medullaris is normal in configuration and location.
IMPRESSION:
1. Postoperative changes at L5-S1 status post intradiscal and posterior fusion with
enhancing right paracentral epidural scar. No significant stenosis.
2. Mild posterior bulging desiccated discs at L3-4 and L4-5 without evidence for nerve
root impingement or spinal stenosis.