Managing Disc Bulge: Effective Strategies for Pain Relief

Do you have a disc bulge that is causing you incredible pain in your lower back?
Does your disc bulge give you sciatica or pain down your leg?
Have you wondered what’s going on in your lower back to cause all this pain?
In this issue of Bodi Empowerment, I go over what’s going on with your disc bulge, the cause of your pain and what kind of treatments are best for you. In other words, I act as a guide to help you decide what to do.
Disc herniations, or disc bulges occur when the disc that is found between vertebrae in the spine is damaged. Most of the time the damage occurs in stages.
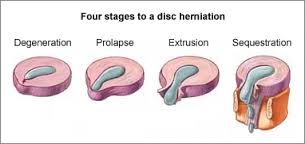
Here are the four stages of a disc herniation or disc bulge:
- Disc Bulge
- Disc Prolapse
- Disc Extrusion
- Disc Sequestration
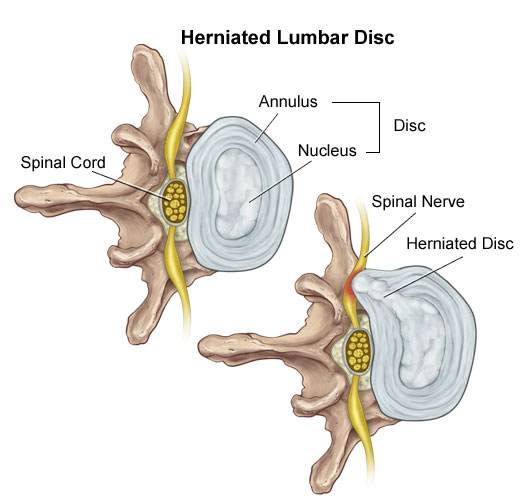
Think of the disc as a flat hard onion with strawberry jelly inside. The jelly is the nucleus while the onion layers form circular layers of hard cartilage called the annulus.
Disc Bulge
If you were to damage the annulus (onion) enough the disc gets to a point that when you bend forward, you pinch the front of the onion so it starts to bulge the onion at the back by pushing the nucleus (jelly) backwards.
This is called a disc bulge. For most of you, there is no pain but for some of you, there can be considerable lower back pain and even sciatica from this small disc bulge.
Disc Protrusion
A disc protrusion is like a disc bulge that comes out even more in one focused spot. The disc pushes out as if you had your finger inside a balloon and pushed out.
Most of the layers of the onion (annulus) have been damaged but the jelly (nucleus) is under considerable pressure. The jelly (nucleus) squeezes through the layers of the annulus (onion) with the few intact layers of the onion (annulus) and the PLL (posterior longitudinal ligament) holding the jelly from spilling out. The disc is still contained by the annulus and PLL ligament. ie the balloon hasn’t popped.
Disc Protrusions usually cause quite a bit of lower back pain and often times sciatica. Many of you, with disc protrusions, on the other hand, have absolutely no pain. There is no clear reason. A study found that 40% of people with no pain whatsoever had disc protrusion confirmed by MRI (Magnetic Resonance Imaging Machine) [1]
The trick is not to let your doctor diagnose you based on just an MRI. An MRI that shows a disc protrusion by itself is not a diagnosis. It’s what a normal person with no pain can have. Make sure there is other evidence!
Disc Extrusion
Disc Extrusion is a disc bulge so large that it breaks through the last layers of the onion (annulus) and the PLL ligament pushing into the area of the spinal cord. ie. The balloon has popped. If you have an extrusion you likely have a tremendous amount of pain leg pain and usually some lower back pain.
Surprisingly when a group of normal people with no pain were scanned with an MRI 18% were found to have disc extrusions (severe disc herniations). [1]
When you have a disc extrusion chances are the extrusion is likely causing your pain as it’s so large.
Disc Sequestration
Disc sequestration occurs when a piece of your jelly (nucleus) that breaks through the onion (annulus) and the PLL ligament has now broken off and moved away further into the spinal cord area. When you have a disc sequestration you have a tremendous amount of leg pain and some lower back pain.
Smaller Is Better: Disc Bulge
Disc Herniations or slipped discs are better if they are smaller, right? You will have less pain right? Yes except when they give you pain. Remember all those normal people with no pain with all kinds of slipped discs? They had disc bulges, disc protrusions, and disc extrusions and even disc sequestrations with no pain.
On the other hand, even with a small disc bulge, you can get a lot of pain and even sciatica with no pressure on the nerve. So smaller isn’t always better.
Bigger Is Better: Disc Bulge
Sometimes bigger is better. Most people like you with disc extrusion and sequestration have lots of pain. The fact is these painful extrusions while more painful usually shrink with time. It takes about a year but with the shrinking of the herniations, the pain does decrease.[2-5]
Disc Herniation: Disc Bulge Treatment
#1 Stop Aggravating Yourself
Half the problem why people don’t get better is that they continually aggravate their lower back and their slipped discs. Learning to lift properly, sit properly and even stand over the sink while brushing your teeth properly can help you avoid the pain.
Even Yoga exercises such as the downward dog can aggravate the lower back, Pilates and even your basic abdominal crunch have been shown by Dr Stuart McGill to increase the pressure in the disc beyond its safe limit.
If you want to find out how to stop aggravating your lower back, click the link below.
See Also: Slipped Discs: Best Self-Treatments To Help Your Lumbar Disc Herniation
#2 Exercise For Disc Herniations / Slipped Discs
For complete instructions on exercises for slipped discs click the link. Best Exercises For Your Slipped Disc
#3 Chiropractic Adjustments For Disc Bulge
A major research paper showed that people who have had lumbar disc herniations who have failed at least 3 months of medical management, including treatment with analgesics, lifestyle modification, physiotherapy, massage therapy, and/or acupuncture, should consider chiropractic spinal manipulative treatment, followed by surgery if unsuccessful. [6]
I would also add that I would try 3 different chiropractors as the competency level varies from person to person. Like any profession including medical doctors and physiotherapists, there are the good ones and bad ones.
See also: 6 Things You Should Look For In A Chiropractic Clinic
#4 Acupuncture For Disc Bulge
Acupuncture is helpful for Slipped Discs in the neck and the lower back.[7-8]
#5 Injections
In a study of two different groups getting treatment for lumbar disc herniations, the group getting chiropractic manipulation had 76.5% of the people improve while the group getting the nerve root injections improved by 62.7%.
After a month, the chiropractic spinal manipulation group had a 60% reduction in pain compared to the nerve root injection group, which had a 53% decrease in pain. Keep in mind the nerve root injection group seemed to be worse to start with compared to the spinal manipulation group.
See Also: Chiropractic Spinal Manipulation Vs. Nerve Root Injections for Lumbar Disc Herniations
Epidural injections are also helpful for lower back pain and the radiating pain down your leg.[8]
#6 Surgery
#1 Discectomy
There are two types of surgery available for slipped discs. Discectomy and spinal fusion. This surgery involves cutting out the piece of the disc that is protruding out and pushing on the spinal cord or nerve.
Discectomy is relatively simple compared to spinal fusion. You have a much better chance of success with discectomy if your MRI shows that your disc herniation is greater than 7 mm thick and correlates well with your neurological exam and nerve conduction studies.[9] If your lower back pain is greater than your leg pain discectomy will not likely work very well for you.[10]
#2 Spinal Fusion
Spinal Fusion removes the disc herniation, jelly (nucleus), and most of the annulus (onion). Bone from the pelvis is then transplanted where your disc was so that the two vertebrae become one.
What Treatment Should You Do?
You should do at least 3 months of therapy when you have a slipped disc before even considering surgery or injections. Start by not aggravating your lumbar disc. You need to modify how you bend forward, lift and even pick up your socks.
See Also: Disc Herniation: Best Self-Treatments To Help Your Lumbar Disc Herniation
If you have trouble sleeping at night you can take painkillers to help you get a better sleep. Don’t stay in bed though. When you have excruciating pain you should only have bed rest for a maximum of two days total.
Next, try chiropractic or physiotherapy with someone who also does acupuncture. Make sure it’s not with somebody who knows how to do 20 acupuncture points. Be patient with them as disc herniations can be difficult to deal with.
Attend regularly 3 times a week for at least a month. Make sure they change the treatments to find what works best for you. If they keep doing the same thing each visit but you are improving that is fine, but if you aren’t improving then it’s time to find a new chiropractor.
If you don’t get any better after a month change to a different chiropractor. I recommend trying 3 different chiropractors as different chiropractors have different training.
If you plateaued or haven’t improved at all then it’s time to get a nerve root injection or an epidural injection. Make sure it’s with a person that does this every day. An emergency room doctor or family physician only does this procedure once in a while. It’s better to get someone more experienced.
When conservative care has been completely exhausted then it’s time to consider surgery. Discectomy is more conservative than spinal fusion and recovery is much quicker. You should consider discectomy surgery if you have :
- Foot drop that is getting worse.
- Any other neurological symptoms that is getting worse like your reflexes, sensitivity
- Bowel or Bladder Symptoms (loss of your poo and pee function). : This is an emergency you should go to the hospital right away.
- If you have a disc protrusion or that is 8 mm or larger that correlates well with a neurological exam, and Nerve conduction tests.
- Leg pain is worse than your lower back pain.
Beware of the surgeon who wants to operate on a small disc bulge. There are too many unnecessary surgeries in the USA especially spinal fusion.
Spinal fusion is considered when your lower back pain is worse than your leg pain
Tell us what you think in the comments below and like us on Facebook. This Toronto Downtown Chiropractor will answer all questions in the comments section.
Research
1. Weishaupt D et al. “MRI of the lumbar spine: Prevalence of intervertebral disc extrusion and sequestration, nerve root compression and plate abnormalities, and osteoarthritis of the fact joints in Asymptomatic Volunteers.” Radiology – 1998; 209:661-666
2. Maigne JY, Rime B, Delignet B. Computed tomographic follow-up of 48 cases of nonoperatively treated lumbar intervertebral disc herniation. Spine 1992; 17:1071-1074.
3. Ikeda T, et al. Pathomechanism of spontaneous regression of the herniated lumbar disc: histologic and immunohistochemical study. J Spinal Disord 1996;9:136-140.
4. Ahn SH, Ahn MW, Byun WM. Effect of transligamentous extension of lumbar disc herniations and their regression in the clinical outcome of sciatica. Spine 2000; 25:475-480.
5. Komori H, Shinomiya K, Nakai O, et al. The natural history of herniated nucleus pulposus with radiculopathy. Spine 1996; 21:225-229.
Research
6. McMorland G et al.Manipulation or microdiskectomy for sciatica? A prospective randomized clinical study. Journal of Manipulative & Physiological Therapeutics 2010; 33: 576-584.
7. Wu, Yao-chi, Jun-feng Zhang, Yi-jun Sun, Cheng-fei Huang, Ping Shao, and Gui-zhen Liu. “Clinical study on electroacupuncture for cervical intervertebral disc herniation.” Journal of Acupuncture and Tuina Science 11, no. 6 (2013): 371-374. – See more at: http://www.healthcmi.com/Acupuncture-Continuing-Education-News/1249-acupuncture-found-superior-to-drug-for-neck-disc-pain#sthash.vD0pNepM.dpuf
8. Wang HeshanNon-Surgical Therapy For Prolapse of Lumbar Intervertebral Disc. The Journal of Traditional Chinese Medicine
9. Parr AT, Diwan S, Abdi S. Lumbar interlaminar epidural injections in managing chronic low back pain and lower extremity pain: a systematic review. Pain Physician 2009;12:163-188.
Research
10. Carragee EJ, et al “Clinical outcomes after lumbar discectomy for sciatica: The effects of fragment types and annular competence” J Bone Joint Surg Am – 2003; 85(1):102-108
11. McMorland G et al.Manipulation or microdiskectomy for sciatica? A prospective randomized clinical study. Journal of Manipulative & Physiological Therapeutics 2010; 33: 576-584.
Related Categories: Acupuncture, Back Pain, Disc Herniation, Imaging, Low Back Pain, Surgery







Hello Dr.
My name is Mini and i am 28,Female
I need an advice on this MRI impression which says Subtotal disc desication is seen with mild generalised disc bulge with small posterocentral disc protrusion at L4/L5 level is causing indentation over thecal sac.
Is it a thing to worry ??
I have a cotinuous lower back pain from 40 days.
Author
Thanks for your question Mini. You need to give me lots of details of your symptoms. If you are not detailed I cannot help.
Hope that helps your possible slipped disc.
History of present illnesses
Past history of fall in childhood at around 12 years of age
I was alright til 2008 when I started having complaint of weakness in both lower limbs.(report not available)
cervical injury C2-C3
Operated in 2008, but after operation I was alright till 1 year. After 1 year, he started having weakness in bilateral lower limb, increased gradually.
At Present
Weakness in bilateral lower limb from waist .
Sensation intact..
No bowel/bladder complaints.
Needs support while walking, I use stick
Weakness in right hand>left hand
Independent in all ADL
Operated for C2-C3 translaminar screw and rod fixation with occipit using occipital T- plate.
MRI (AAD with C2-C3 and C4 disc bulge withy focal canal stenosis.
Author
Thanks for your question Mahesh. You have too much pressure on your spinal cord in the neck affecting your lower limb. Likely something happened with the operation but I cannot say for sure. Or you have developed a disc herniation below, above the area where you were fixed. This is not uncommon. Either way I have not way to determine this. You will have to get another opinion from someone that can examine you. This is not the right forum for your problem.
pls help. me. m facing this from 1yr. no one. Doc is able to find what is exact problem. why m getting pain in Lower back nd below the chest
m showing U my MRI report.
it shows l4-l5 asymmetrical diffuse posterior buldge with left forminal annualar tear without neutral compromise
my xray report was normal.
where should I go? I already gone for neuro, physio, ortho. no one is able to find what is exact problem
Author
Thanks for your question Farheen. You need to give me a lot more details about your symptoms Not MRI reports. Even your MRI reports don’t have enough detail. I cannot help you based on what you have written.
Good luck with your slipped disc.
Hi Dr. Ken Nakamura. I am 28 years old, a nurse with 4 years experience in a hospital. Last May 27, I experienced moderate low back pain with the scale of 7/10 which radiates to my lower left leg. The pain is excruciating and it worsen when I stand or sit for a long time. Even walking for a mile is painful. I was prescribed with Gabix, a gabapentin which I should take once a day at bedtime. The pain wasn’t relieve so I decided to file a sick leave. Our rehab doctor advised me to take an MRI of my thoracolumbar.
The result of my MRI is disc dessication and disc bulge of L5-S1. I was a bit confused because the pain sometimes subsides then when it came back, it’s much worse than before. I had difficulty sleeping because of the pain especially the tingling and numbness that radiates on my left leg. Pain relievers such as celecoxib doesn’t relieve the pain.
I just want to ask is it really possible that my diagnosis is just disc bulge? The MRI says it’s just mild so my rehab doctor is puzzled because of the pain i’m experiencing. I want to have a second opinion of my MRI because of pain. By the way, the pain usually occurs at night time.
Thank you in advance
Author
Thanks for your question Marlyn. Which position do you sleep. If you sleep on your side do you curl-up like in the fetal position or do you keep the legs straight do you extend them.
Let me know your answer.
Sorry for the late reply. I usually sleep on my right side cuddling a pillow, most probably in a fetal position. As of now, the pain on my lumbar area is not that painful unlike before and it only attacks when I’ve been sitting or walking for too long. Though the numbness on my left leg is still present even at rest with pain scale of min 6/10 max 7/10.
Thank you Dr. Ken
Author
Thanks for your question Marylyn. First you should know that most MRIs are taken while lying down. Your pain is there when you sit. We know that the disc pressure is much higher when you sit and stand compared to lying down. So MRIs in general do not give you a true representation of your problem. A diagnosis is not by MRI it’s by a careful history and examination. An MRI shouldn’t be used very often for lower back pain. Trauma, suspected cancer, infection, suspected pars fracture (fracture of the spine) etc… are times to use them.
First try doing knee to chest exercises checking your range of motion (ROM) before and after and seeing how you feel before doing the knee to chest exercises. You lay on your back with your knees bent and your feet on the floor. Bring your knees to your chest as far as the knees will go or until you feel tightness in your lower back. Stand up and check your ROM again. If you are worse than stop the exercises. If you feel better do the exercises 4 times a day.
Hope that helps your likely disc herniation.
Thank you so much Dr. Ken. My Physical Therapist also did a straight leg raise test on both of my legs. My left leg can only be bend at 60 degrees because of the pain. I also did the knee to chest exercise you’ve said and i felt the numbness on my left leg after doing it for 2 counts.
Last night, I slept on my left side and i felt the pain on my left lumbar area with pain scale of 7/10. Unlike before that the pain is on the whole lumbar area. Our orthospine diagnosed me with possible neeve irritation and will do a nerve block after a month of Rehab. But I was quite unease about his diagnosis. Do you think I should undergo a nerve blocking or consult another doctor?
Sorry for asking too many questions. I was just anxious about my situation. Thank you so much.
Author
Thanks for your answer Maryln. So are you saying you are better from doing the exercises or for another reason? If that is the case just keep doing the exercises. If not let me know.
Hope that helps your slipped disc.
Good Day Ken Sir,
I have read your article and felt i get a better solution and information.
My mom has a neck pain from last 8-9 months, In beginning its very little bit, but as time passed its growing,
When we consulted with Doctor , first he consulted for X-ray but no result. then he consulted us to MRI.
now he said its normal, dont worry too much, he gave some medicines for 15 days but there is no any relief , after 15 days he again changed medicine but no result still, and now we are very worry about it, Still we have no clear information about this, hence we request you to help us.
Now i m writing whatever in report ”
MRI Cervical Spine
Sequences obtained using A 3 Tesla Siemens Magnetom Spectra MRI Scanner :
Cervical Lordotic curvature is straightetened. Vertebral bodies are normal in morhology and marrow signal. Degenerative changes are seen in form of tiny marginal osteophytes formation at multiple levels.
Posterior disco-osteophytic bulge are seen at C4-5 C5-6 and C6-7 levels indenting anterior thecal sac.
No significant disc hermiation seen at any level. Spinal cord shows normal morphology & signal intensity with no obvious abnormal focal/diffuse lesion.
Spinal canal diameters at various disc levels are as follows
C1-C2 (11.2 mm)
C2-C3 (11.7 mm)
C3-C4 (11.5 mm)
C4-C5 (10.9 mm)
C5-C6 (10.7 mm)
C6-C7 (11.2 mm)
Cervico- medullary junction is normal.
all of above has written in report……… Dear Sir , please revert as soon as possible and advice for being better as possible.
Author
Thanks for your question Tilak. You are asking for a diagnosis. I don’t make diagnosis over the internet. Also keep in mind a diagnosis is made by history and exam and not imaging like MRI. In addition there is nothing on MRI that shows the cause of any pain as more people over 40 years of age there is degeneration.
I would get a second opinion from a different medical doctor. One that will ask extensive questions regarding the situation.
Hope that helps your mother’s neck pain.
Dear Dr. Ken. I’m from India and a 38 year old male. My job is mostly in front of the laptop. Thank you for this informative article. For the past 3-4 months, I had a moderate pain on my left hand especially on the elbow and shoulder. Initially I thought it was because I was lifting my three year old son always with my left hand. Then I stopped lifting him for almost 2 months and avoided lifting anything heavy with my left hand. But the pain did not go. It feels a bit more painful in the night but still bearable. The pain persist throughout the day. I consulted an orthopedic surgeon two weeks back. He took a X-Ray but nothing could be found. Did a blood test and it had creatinine on the upper border lines. Now, for the past one week, the problem on my left hand got a bit worse. I started having a persistent tingling sensation right from the edge of my thumb finger to the elbow of my left hand. It is there almost all the time. Yesterday I went to see a Neuro physician and after some physical examinations he suspected there may be a compression on the cervical disc causing this. He ordered a MRI scan. The scan report says the following among other things: “straightening of the normal cervical lordosis is seen. Left paracentral extrusion of CV5-6 IV disc is seen indenting thecal sac and causing compression over left exiting C6 nerves. Mild posteriocentral protrusion C6-7 IV disc indenting thecal sac. No other significant disc bulge/herniation is seen. Spinal canal is adequate in size…. ” The Neuro surgeon, after another round of X-Rays of cervical spine, told me that it needs to be operated. According to him, surgery will provide a permanent solution to the problem. He also advised wearing a cervical collar.
I would like to know if surgery is the only option. Would conservative treatment suffice? If surgery is the only option, how serious is the surgery and what are the possible risks involved? Thanks for your advice.
Author
Thanks for your question John. You always do conservative therapy first unless it’s urgent. Urgent means that you have muscles that are wasting that is getting worse all the time. It sounds like the MRI and your symptoms correlate well meaning that your C6 nerve is causing your pain. You should see the best available chiropractor or best physiotherapist in your area.
Surgery is quite complicated in the neck much more so compared to the lower back. Also depending on the type of surgery I don’t know it to be a permanent solution in many cases. It may be with some. Has the Neurosurgeon followed up with all his patients 5, 10, 20 years. The answer is no. He actually doesn’t know the answer to that. Think about it. Anybody that tells you it’s a permanent solution from my point of view I would regard with a little scrutiny.
Provided this surgeon said this I will tell you that there are no guarantees with any treatment. Did the neurosurgeon actually say that? Do we have a translation problem here? You can look up the risks of cervical disk surgery.
Remember I haven’t examined you or taken a proper history although you have provided quite a good amount of information. That’s just my opinion from the information you have told me. This can change if I have more information.
Hope that helps your cervical disc herniation.
Thanks Ken for your prompt response. I was seeking opinions from various quarters and pretty much every one converges on the point of conservative treatment before a full blown surgery. I guess I will follow that.
Thank you once again.
I am pund, Actually I am getting half body sweating alternatively on left and right. I had been to neurologist but no body is giving correct answer, I have took MRI for brain and cervical spine, nothing was problem. In cervical report it says mild cervical spondylotic changes with a posterior central and left paracentral subligamentous disc protrusion at c6-7 level resulting into left neural canal and neural foraminal compromise.
doctor suggests this is not the cause for half body sweating, please let me know
Author
Thanks for your question Pund. I have never seen anybody have body sweating to half their body due to a disk herniation. Usually the autonomic nervous system is not functioning properly. Sometimes you are born with it and it activates or is triggered to happen. I don’t think anybody knows the real cause. That’s just what I have read. It’s definitely not related to the disc.
Hope that helps answer your question regarding your disc herniation.
v
Spin Echo T1w and fast spin echo T2w high resolution saggital images of lumbosacral . spine were obtained on a dedicated phased array surface spine coil. Using 1.5T high gradient MRI systems and correlated with T1a dn T2W Axial Images.
Findings:-
Early spondylotic changes are seen in the form of small marginal osteophytes, facetopathy and multiple levels partical disc desiccations in form of reduction of high signal intessity on T2W images.
Diffuse disc bulge at L4-5 level, impinging upon the thecal sac and bilateral descending L5 nerve roots with mild bilateral nuro-foraminal narrowing.
Diffuse disc bulge at L5-S1 level, impinging upon the thecal sac and bilateral descending S1 nerve roots with mild bilateral nuro-foraminal narrowing.
No significant dis bulg/protrusion is seen at any other level.
Distal cord, conus medullaris and filum terminale are normal in MR morphology.
Pre and paravetebral soft tissue are normal
Bony spinal canal is capacious at all levels
Posterior spinal elements are normal
Bilateral psoas muscles appear normal with no collection seen
Bilateral sacro-illac joints appear normal with no evidence of any active sacro-ilitis seen
I have sitting job in computer daily as routing work 8-10 hrs ist time this pain suddenly come in low back in sitting position but not in walking running etc. i hv taken or seen it 3 orthomadic dr he given me medition after taken it get relief but when it finish then slow slow pain come against or i get deprician more by this. give me best suggestion now some more improvement the last in sitting but in whole day working in evening time my back tired . my pain is not in my legs.
Dr sir please give me your best suggestion. as per your suggestion it will be done ok or not i am 42 age. this problem was not before any day to me its come suddenly last 4-5 months
Author
Thanks for your question Pankaj. You should try these exercises. https://www.bodiempowerment.com/herniated-disc-part-2-the-best-exercises-for-your-herniated-disc/
The exercises have to supervised by a chiropractor or physiotherapist in your area as they can make you worse and they need to modify the exercises when needed.
Hope that helps your disc bulge.
Dr ken sir i hv written u last 2 month now i m getting some better relief before 2 month my position was problem is sitting 8-10 hrs that was very tuff but now its improvement 80% sir can i do morning walk secoundly now my back point pain in less but as passed day evening time my feel in low back as jakran i want smoth it how can i do it does surgery in best option for that pls give me some more suggestion dr sir also i hv gastic problem i hv sitting job in office around 9-10 hrs
Author
Thanks for your question Pankaj. If you are 80% improved why would you even consider surgery? Surgery can make you worse, better or have no change at all. You can just do the extension exercises similar to the cobra in the link: https://www.bodiempowerment.com/herniated-disc-part-2-the-best-exercises-for-your-herniated-disc/
The only difference is you should breath out once you reach the top. Also, you try and go further each time.
Hope that helps your disc slipped disc. Also, buy yourself a standing desk.
Thank u dr sir your good responce i will written u again
Author
You are welcome Pankaj.
Hello,
Dr Kin, i am faheem from punjab multan, pakistan. I have lower bach pain from many years but it is fine after a few hours rest. 10 month ago during my house shifting i lift weight and from then my back pain was worse.. Itstarted getting fine after several nonths, but 3 months before during exercise i once again got some problem. Now there is nimbness and butning feeling in my legs and fingers mostly right side, and back pain if i walk longer or sit for more than 15 minutes,
My mri report is
Retrolisthesis of l4 over s1 and disk decicatory change with central disk protrusion at l5-s1 causing thecal sac indentation with mild circumferential disk bulg at l4-l5…
Plz advice me better treatment and exercises…
Regards, faheem
Hello, Dr.Ken, i have pain in my back when i bend forward. i thought it was because my spine was bent forward.But when i consulted orthopeadic doctor,
he checked if i have any problem with my legs. my legs are fine and no numbness/pain. he asked me to get x-ray which turned out to be normal. the conclusion of MRI report of lumbar spine is “diffuse annular bulge at L4-L5 and L5-S1 levels,causing mild thecalsac indentation”
Seeing the report , doc said that the discs in my neck and spine are degenerating which can be seen in MRI as darker in neck and also near L4-L5 AND L5-S1. he said that i’m a young(22) guy and the discs can regenerate if i do physio excercises everyday and play sports like swimming,soccer,etc. he said it might take minimum 6 months to recover. what do u think? will i be able to recover? would u suggest any excercises that will benefit me?
Author
Thanks for your question Ajay. First I’m curious you paid or some insurance paid for the X-rays and MRI is that correct?
Helo sir i am Dinesh from Punjab . I have pain in my left leg from four months in walking time . I am anot able to continew walking . I go for phisioythrepy for 10days resguler also . I take medicens also . I take medicens form orthopedics also . He sugest me for mri.in mri my peroblem is diffuse disc bulge with left paracentral disc protrusion at L4-L5 level indenting of thecal sac and bilateral L5traversing nerve roots.. I do exercises also but some some time peroblem increse and some time decrease. I am confuse wht type of treatment beter for me. Now Dr sugest me nerve injections. Please advise me why type of treatment beter for me. I am able to walk but I have to stand for two three seconds when pain is increase. Sugest me exercises also if peroblem is able to solve with only exercises.
Author
Thanks for your question Dinesh from Punjab, India. Sounds like a solid recommendation to do injections. After that I would follow-up with the best physiotherapist or chiropractor in your area.
Hope that helps your slipped disc.
Dr. Ken from Toronto
HI Dr. ken,
Below is my MRI report,
Clinical history:
Lower back and both legs pain more on left side.
Study protocol:
A plain MRI of the lumbosacral spine was performed.
Sagittal-T1,T2, STIR, coronal-T1, STIR, T1 weighted sequences. Previous MRI is available for comparison.
Contrast details:
Nil.
Findings:
Normal alignment and curvature are maintained. The vertebrae show normal marrow signal. The posterior elements appear normal.
The L5-S1 disc is degenerated with moderate posterocentral disc protrusion indenting the thecal sac and traversing nerve roots.
Mild diffuse bulges are seen of the L4-L5 disc indenting the thecal sac without significant neural foramina compromise.
Rest of the discs appear normal.
The conus is normal.
The perivertebral soft tissues do not show any significant abnormality. The pre and paravertebral soft tissues appear normal.
The sagittal bony canal dimensions are within normal limits.
The ligamentum flavum, facetal joints and other neural foramina appear normal.
Both sacroiliac joints are normal.
Impression:
The L5-S1 disc is degenerated with moderate posterocentral disc protrusion indenting the thecal sac and traversing nerve roots, no significant change from previous MRI.
Mild diffuse bulges of the L4-L5 disc indenting the thecal sac without significant neural foramina compromise.
please advice
Author
Thanks for your question Sahil. You need to write just as much detail about your pain. An MRI is not a diagnosis it’s a tool that’ s often misleading. I cannot help you unless you are very explicit about the details regarding your pain. Lower back pain and leg pain just not enough information. Please note if you write a couple of lines I will not be answering you.
Hope that helps your slipped disc.
hi Dr. ken,
I have been experiencing a lower back from the last year which was going into my legs (no tingling) as well. In April last year I decided to see orthopaedic , at that time my Vitamin D was also low so he gave me medicines for vitamin D as well. After few rounds In July he recommended me to go for MRI. After reading through the report (the above report is latest report and not the last year’s report) he advised me to go for the surgery to which I refused. Later I went for physiotherapist, she did tens, IFT, tractions, ultrasonic massage session for 5 days and told me to do exercises this was in August 2015. later I went for my job in another city, I was continuously doing exercises she told me on daily basis but I was still experiencing pain in back and legs (both). I decided to take second opinion. So, in March 2016 I went for another orthopaedic showed him the reports and explained the background. Because of my deficiency in vit. D he recommended latest vit. D test, the report came normal. His physiotherapist told me few exercised and there were 2 session of Matrix rhythm therapy. I was advised not to ride a bike, wear belt while sitting (I have a 9-5 sitting job ) ,traveling, keeping right posture and exercises (theraband exercises). There has been some improvement but I am not able to recover fully. My current situation – I have a more pain in the lower back left side than on the right. And at times the pain goes into both legs till calves (sometimes till ankle) and back of thighs. I strongly feel that if I sit for longer durations I experienced more pain in my legs those days. Last week my orthopaedic told me he wants to see latest MRI, the report I copy pasted in last message was the latest one. The observation in report is same as that of my last year’s report but there has been some improvement over the last year. I do feel good after exercises but it has been 4-5 months of exercises now and I am not able to recover fully. This is very frustrating. Please advise.
Author
Thanks for your question Sahil. You should try these exercises. https://www.bodiempowerment.com/herniated-disc-part-2-the-best-exercises-for-your-herniated-disc/
These exercises should be done under the supervision of a chiropractor or physiotherapist at least initially as you can get worse. You may have to increase or decrease the frequency of the exercises according to how you respond. The exercises may also need to be modified, thus the reason for you to consult a chiropractor or physiotherapist before doing the exercises. Do not them with their guidance.
Hope that helps your slipped disc.
Thanks for your advise 🙂
Author
You are welcome Sahil.
hi Dr,. Ken,
I had an appointment with my orthopaedic today, he compared both the MRI reports- last year’s and the recent one I pasted. I told him that though the impression in both the reports are same, I do feel some improvement over the last year. He verified that in the reports -confirming less protrusion now. He recommended traction now for 4 days 8 hours each. Just want to have your view point on this. Should I go for traction? Or mere changing the exercises would be more beneficial. Please advise.
Author
Thanks for your question Sahil. Sounds like constant traction which I never recommend. The problem with constant traction is after getting out of the traction machine you can be much worse. With intermittent you will know right away and usually you won’t get significantly worse. That’s just my opinion and not based on solid research.
Hope that helps your slipped disc.
Sir I am manoj saxena from Lucknow,uttar Pradesh, India. I had mild back pain and severe leg pain in 2004 at the age of 34 .Even painkillers could not provide me relief.then I went to the doctor and he examined me,my left leg could be lifted only up to 40°. He just told me that it is chronic position and advised complete bed rest and MRI report. MRI report showed the following-
1. Degenerative L4-5 invertebral disc.
2. L4-5 disc shows posterocentral protrusion causing thecal indentation and bilateral exit neural foraminal narrowings.
3. L3-4 and L5-S1 discs show posterior flattering causing mild thecal sac indentation and bilateral exit neural foraminal narrowing.
As per doctor I did the complete bed rest and advised excercises and became fit in about 6 months. Now I have reached the age of 46 and now am suffering with pain in left leg from buttock to toe Since last 6 months. On april 15,2016,I felt numbness in toe ofnleft leg. I just went to the doctor and he advised me bed rest and gave me some steroid pills,etc and I got some relief in pain and numbness in the toe went out completely. But by taking steroid pills I had much stomach pain, swelling in intestine and other gastric problems. So the doctor stopped giving me steroids and advised for rest,MRI and metycobalamin injection of wockhard company. On 17 may ,2016 I did MRI and its report is as follows-
1. Lumbar spinal curvature is maintained. Vertebral bodies are showing normal height,alignment, curvature and marrow signal intensity pattern. No obvious inflammatory or infective pathology is seen.
2. L4-5 intervertebral disc is degenerated. Diffuse disc bulge at L4-5 with posteocentral disc extrusion associated with annular tear with mild inferior migration indenting the thecal sac and bilateral lateral recesses. Ligamentum flavum is thickened at this level with facetal arthropathy at multiple levels.
3. Lower dorsal spinal cord and conus medullaris are showing normal morphology, outline and signal intensity. No evidence of primary canal stenosis.
4. Pre and para vertebral soft tissues are normal.
By seeing report my doctor said that its final treatment is only operation and referred my case to a neuro surgeon.
I have pain in left leg from buttock to toe while walking and standing. While sitting I have to adjust my leg and then I don’t feel much pain and while I am on bed I don’t feel much pain. But when I get up from bed I feel some weird sensation in the left leg for a minute. I am still taking rest and till now I have taken 8 injections of methycobalamin in 16 days. Now I am taking tolperisone hydrochloride JP 450mg, flupritine maleate 300mg, ranitidine hydrochloride JP 300mg, gabapentin 600mg per day and I am also doing spinal excercise.
I don’t want to go for the operation. I am in a touring job and use to travel in car,bus train for long distances. Please advise me that what should I do and how much time I need to do the rest. If I start to do journey by taking painkillers, etc then can the problem of neural damage arise. Please! Advise me the best as soon as possible.
Author
Thanks for your question Manoj. You should get another opinion but really in your case the operation would likely be more helpful. Exercises will likely make you worse. Not everybody can be helped by exercises. Your case is too severe.
Hope that helps your slipped disc.
Dear Doctor,
Thank you for this platform. I have been suffering lower back pain followed by leg pain since last 3 years. Some time pain spread between shoulder and lower back. Now I am suffering severe pain on my lower back and leg pain.
MRI reports says ” Diffuse disc bulge at L5-S1 causing mild impression on thecal sac”. I had a blood check result about RA Factors and It seems normal. I had consulted to a Nuerologist.
I would like to know whether this pain can be cured with exercise or Medication.
Author
Thanks for your question Shanavas. You can do these exercises. https://www.bodiempowerment.com/herniated-disc-part-2-the-best-exercises-for-your-herniated-disc/
I cannot verify for your diagnosis. However these exercises may help but they may make you worse. These exercises should be done with a health professional that has experience with these exercises at least at the beginning. If the pain, numbness or tingling gets worse or goes further down the leg than you are getting worse. You should then stop the exercises.
Hope that helps your possible slipped disc.
Hi my Marla,
I am impressed by your site amd truly appreciate that you have this for people like myself to get answers to our questions.
My question to I was seen at the ER on June 14, 2016 And the findings were a trace of retrolisthesis L1-L2 And) L2-L3 with slight disc narrowing L5-S1. Sacroiliac changes. WE diagnose was disc disorder intervertabral lumbar with radiculopathy. What treatments should I look for from my doctor and is a an injection suppose to be put in the arm or buttock area? I had an injection as well and it was put in my upper right arm and in was prescribe prednisone for five days with naproxen for pain and inflammation. Are these prescriptions usually prescribe for this type of problem. I thank you in advanced for your time and help on understanding what to do with this new problem in my life.
Author
Thanks for your question Maria. You need to tell me your symptoms in detail like all the things that make it worse and better like sitting, standing walking etc…wher the pain is. You’ve only told me what the doctors and what they did for you but not what you feel with your symptoms. I can’t help you until you give me a lot more detail about your symptoms.
Hope you understand whether it’s a slipped disc or not the details are important.
I had the back pain in left leg from last 5 years but now from January 2016 are more then regular
Now I have done MRI and report is on hand.The result is,
There is straightening of normal lumbar curve suggestion muscle spasm. Diffuse disc bulge is seen at l5-S1 level causing bilateral exit canal stenosis and never root compression. Diffuse disc bulge more towards left side with annulus tear is seen at l4-l5 level causing left exit canal stenosis and nerve root compression. Ligamentum flava are hypertrophied at L4 – L5 and L5 – S1 levels. Pre and para vertebral soft tissues are normal.
So pls gave me a good suggestions to solve my problem forever.i have been used a lot of painkiller tablets and injection .
So now I need ur advise
Author
Thanks for your question Shakir. https://www.bodiempowerment.com/herniated-disc-part-2-the-best-exercises-for-your-herniated-disc/
You can try to do these exercises with the guidance of a health professional with knowledge of these exercises. If the pain, numbness or tingling gets worse or starts going further down the leg than you are getting worse so must stop the exercises immediately.
Hope that helps your slipped disc.
Hello Dr. Ken,
My English is poor but m trying my best to explain you everything .
15 May 2015 -Back Pain in my Spine,it was before from last 6 months but heavy pain starts from 15 of May 2015
Then on 31 June 2015 MRI Done,
TB Deducted in Spine As a potts Spine
Location of TB:-D11,D12,L1
& 9mm Stone in GB by ultrasound
then Starts ATT from 1 July 2015
Then very high pain start at night time after 40 days of starts ATT.
Then even m not able to walk or stand of because of pain .
Then i was taken completely bed rest for 4 months as per doctor Suggestion
Then after all the pain goes off and i feel relax now from 20January 2016
but on 13 Feb 2016 CT scan show that D11,D12 bone are very week & bacteria eaten too much of that place bone.
Again as per Doctor take some rest to recover that bone and eat some calcium/vitamin diet.
now it’s April 2016 Again CT Scan showing
There is evidence of increased density/sclerosis of D11 and D12 vertebra is seen with osseous
endplate destruction. Bilateral paravertebral and prevertebral collection is seen at D10 – D12
vertebral level. Foraminal collection is seen at D11-12 level obliterating neural foraminas. Left psoas
absces is seen extending from L1 to superior endplate of L4 vertebra measuring 5.9 x 5.2 x 8.1 cm in
size.
Posterior disc bulge is seen at L5-S1 level indenting anterior thecal sac.
As compared to the old MRI dated 19/01/2016, There is progression of size of left psoas abscess
whereas left paraspinal collection shows resolution.
now what i have to do …..???
There is no pain Now even i can walk properly no issue with walk,
Never tried for journey ..Like bike ,Car,train,flight,Auto or any kind of journey from the last 10Months
if m trying to lift any above 5kg weight then there is a pain in Spine by walking there is no pain till now
Can i go for travelling by Bike,car,Train or should i have to still take rest as per Ct Scan result ????
Author
Thanks for your question Anwinash. Your problem of tuberculosis or TB is outside of my scope of practice. Although I can treat people with lower back pain that happen to have say lung TB that is coincidental your problem is more complex. Your pain can be coming from either the TB or the disc herniation.
I cannot make recommendation for a problem that is outside of my scope of practice.
Best of luck with your TB and herniated disc.
Sir,
I am Priyadharshini
I have lower back pain from past 2 years only on mensus time February onwards pain would be high continuously so I consult doctor and he take some blood test. the report is ESR: 1/2 hours (13mm)
1 hour (30mm)
ASO: Negative
CRP: Negative
RAF: positive ( 1:32 | u/ml)
And also he takes MRI scan on another day. The report is Disc dessication noted at L4-L5 IV disc level.rest of the four disc having normal height and signal intensities.
L3-L4: diffuse disc bulge causing mild anterior thecal sac intendationintendation without neural compromise.
L4-L5: diffuse disc bulge with posterior central causing spinal canal stenosis and bilateral neural foraminal stenosis leading to intendation over bilateral traversing and exciting nerve roots ( left > right)
Degenerative disease of the spine and lumbar disc disease with neural compromise.
So that he suggest me to do physiotherapy after that now he inject steroid injection on my disc L3,L4,L5. And now 20 days are completed after the steroid injection. But my pain didn’t reduce now itself. My leg pain also more severe than lower back pain.
Author
Thanks for your question Priyadharshini. If you only get pain during menstruation than that is a functional problem usually unrelated to the lower back. Usually that is treated medically with pain medication and nutritionally or with herbs by a Naturopath. Usually most doctors would not take an MRI unless something more is suspected.
I would go to your medical doctor for medication or if you want to do a more natural approach a herbalist or a Ayurvedic practitioner.
Hope that helps your lower back.
Thank you for your reply sir,
After steroid injection is it possible to go to naturopathic..and also I get regular pain now. I can’t able to sit for 1 hour continuously my pain gets started. I get fear about my studies. Now I have a pain from thigh to leg. Past three days I taken this below tablet:
Litmus-20
Ebov 90
Dozt-6
Now My leg and hand gets more weight than usual. I have fear about this…
Is there any permanent solution for my disc bulge problem
Author
Thanks for your question Priyadharshini.
This is what you said previously:
“I have lower back pain from past 2 years only on mensus time February onwards pain would be high continuously so I consult doctor and he take some blood test.”
I think I misunderstood you. I originally thought that you only had pain during menstruation time that was continuous only during your menstruation. Now you are saying you get pain after sitting for more than an hour with pain into the leg. So it started off during your period and has progressed to being more progressive with pains into your leg.
It can be either problem at this point with the information I now know so I am not going to recommend any exercises and make sure you have a clear diagnosis and go to your medical doctor as a follow up.
Hope your pains get better.
Yeah sir I consulted so many doctors he suggested to follow up the pain killers only. I need permanent solution sir because now I can’t able to tolerate my pain. Now I have pain in slightly above lower back when I sit I felt something going to break. I only felt ok when I lying on bed. I get fear sir my buttock also get pain rarely at the time my heart gets more tight. Is there any relation between tighten heart with back pain sir. Tablets which I am following are already mentioned in previous reply. Please tell me sir is it serious problem and also many of them are suggested me to go to Mysore for this treatment. But my family situation are poor I can’t able to spend more money. So I get confused. Is it necessary to go to Mysore “rahman bone centre” please tell me, Is there I am in any critical situation sir?
Please tell me may be what kind of problem I have..
Author
I cannot help you Priyadharshini. Your pains keep changing and evolving over time so I cannot be clear without an exam. Also the language barrier seems too great.
Dear Dr. Nakamura,
After a few months of inactivity due to shoulder surgery, I started hiking again (my sport of choice is cycling 30-40 miles/day). After about 7 consecutive days of hiking 4-5 miles, I got a little “twinge” of pain in my lower back on the last hike. I went home right away and iced it. The next day, I was doing some gardening, and got a really big sharp pain as I bent over. This got progressively worse and I ended up in Urgent Care with a 10 out of 10 pain scale.
Long story short,it took awhile before anyone took me seriously and I recently got the results back from my MRI:
HISTORY:unremitting lumbar radiculopathy BACK PAIN, >6 WKS DESPITE
CONSERVATIVE TX
COMPARISON: None available
PROCEDURE: Noncontrast enhanced, multiplanar, multisequence images
were obtained through the lumbar spine.
FINDINGS: Five nonrib-bearing lumbar type vertebrae are present. If
surgical intervention is planned, then plain film correlation may be
obtained.
Conus terminates at T12-L1. Cauda equina is normal.
There is mild levoscoliosis of the lumbar spine centered at L3-L4.
Moderate disk degeneration and height loss is seen at L2-L3 and
L3-L4. Remainder of the intervertebral disks demonstrate normal
height and hydration. Marrow signal is within normal limits.
T12-L1: No canal or foraminal narrowing.
L1-2: No canal or foraminal narrowing.
L2-3: Circumferential disk bulge asymmetric to the left foraminal
region with mild bilateral facet and ligamentous hypertrophy.
Resultant moderate left and mild right foraminal narrowing without
canal stenosis. Moderate left lateral recess narrowing.
L3-4: Circumferential disk bulge with more focal right lateral
recess extrusion and bilateral facet and ligamentous hypertrophy
results in moderate right and mild left foraminal narrowing. There
is mild canal stenosis with mild left and moderate to severe right
lateral recess effacement.
L4-5: Bilateral facet and ligamentous hypertrophy with mild
foraminal narrowing bilaterally. No canal stenosis.
L5-S1: No canal or foraminal narrowing.
No pars interarticularis defect is present. Paraspinal soft tissues
are normal. Visualized extra vertebral soft tissues are grossly
unremarkable.
Sacroiliac articulations are within normal limits. .
IMPRESSION:
1. Lumbar levoscoliosis and degenerative changes predominantly at
L2-3 and L3-L4.
2. L2-3 asymmetric disk bulge resulting in moderate left foraminal
and lateral recess narrowing with possible impingement of the left
L2 and L3 nerve roots.
3. L3-L4 asymmetric disk bulge with more focal right lateral recess
extrusion resulting in moderate right foraminal narrowing and
moderate to severe right lateral recess effacement with possible
impingement of the right L3 and L4 nerve roots.
My pain, after 6 weeks and some analgesics, is now 5-6, primarily in my lower back but occasionally down the from of my left thigh. I have been advised to start light exercising again and PT. I am also doing some recommended stretches at home daily. I just got the MRI results today so I haven’t done much rehab yet.
Would you give me your opinion on whether or not this is a good course of action to follow at this point, if you have any experience with others who have had similar spinal abnormailities and their progress, and if any of this is potentially serious and, without treatment, will eventually limit my mobility? If it helps to know, I am a 58 year old female 5’4 115#.
Thank you,
Susyn
Author
Thanks for your question Susyn the SportyGirl. You are doing pretty well considering everything. I would do the exercises recommended in this article. However I would imagine that your physiotherapists have already given you these exercises. Alternatively you can find yourself the best chiropractor in your area to help you out. Here is another article to help you out. https://www.bodiempowerment.com/herniated-disc-part-2-the-best-exercises-for-your-herniated-disc/
Part 1 is also good.
Just in case, if the pain, numbness or tingling starts going down into the buttock or the leg you are getting worse. You should stop the exercises at that time as the exercises are not for you.
Hope that helps your slipped disc.
disc desiccation with diffuse disc bulge at l5-s1 level showing annular tear causing mild bilataral lateral recess stenoses What should I do
Author
Thanks for your question Shakeel. You need to write lengthy details about your back. A snippet of your MRI is not helpful.
Hope your understand you need to give a lot more detail about a possible disc bulge diagnosis. An MRI is not a diagnosis.
sunil
i had back pain from last two month i done MRI LS Spine on
below the MRI result any problem in my dics in L5 and 4
Examination– MRI L S spine
there is loss of lumber lordosis with straightening if spine.
L5-s1 lumber intervertebral disc exhibit signal changes- S/O partial desiccation.
small dorsocentral focal bulge of L5-S1 disc is noted indenting the thecal sac.
annular bulge 0f L4-5 disc, abutting the thecal sac this is the sleep disc problem.
no significant facetal degenerative changes or ligamentum flavum thickening.
rest of the intervertebral disc in height, contour & signal characteristics.
Lumbar Canal diameters at disc level are as follows.
L2-3—–17 mm.
L3-4—–14 mm.
L4-5—–13 mm.
L5-S1—-12 mm.
The vertebral bodies are normal in height, morphology and signal characteristics.
no evidence of spondylolishesis.
no abnormal per or paravertebaral soft tissue
Impression
loss of lumber lordosis with straightening if spine.
.small dorsocentral focal bulge of L5-S1 disc is indenting the thecal sac.
annular bulge 0f L4-5 disc, abutting the thecal sac
No evidence of infective focus in the spine .
pls replay me
Author
Thanks for your question Sunil. I can’t help you without you telling me what your symptoms are. Tell me where, and what makes it worse, better etc… Write a at least 2 paragraphs about your pain. Your MRI is not the important part your symptoms are more important.
Hope that helps your possible slipped disc.
Doctor i don’t have leg pain or hand pain only back pain in one side and lower back pain
from last 2 month
Author
Sunil you need answer my questions. If you don’t answer them I can’t help you. It’s like going to the your medical doctor not answering your doctors questions and repeating that you have back pain. Your doctor or I can’t help with such little information. The MRI is not a diagnosis. It’s only a small part of the picture. Your MRI may say disc herniation, disc bulge or disc extrusion but the history and exam is what leads to the diagnosis. Most of the time a diagnosis is made without an MRI.
Also if you are from India private doctors will send you for an MRI and recommend surgery without conservative care. Unless it’s a emergency situation that’ s quite simply wrong.
Hope you understand I need information to help with your possible disc herniation.